Case Study: Pressure Ulcer Performance Improvement Plan
As part of its QAPI, NuCare Services, operators of 26 skilled nursing facilities in Illinois, Wisconsin, and Arizona, implemented a PIP program focused on facility-acquired pressure ulcers.
PIP team members: Wound care physician, director of nursing, administrator, wound care nurse, treatment nurse, unit managers, certified nurse assistants (CNAs), dietary, and social services.
Root-Cause: Communication
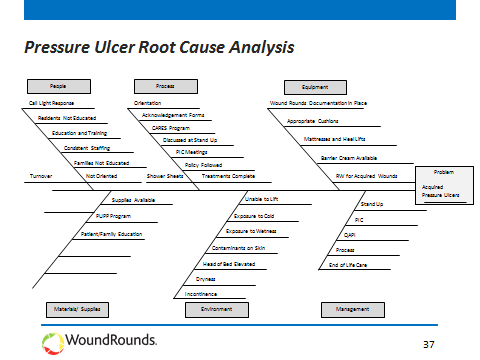
PIP Team members conducted a root-cause analysis, resulting in a fishbone diagram (see below). Other staff input was solicited via a storyboard posted in the break room.
Communication was identified as a root cause to the problem, since CNAs were not always informed about which residents had pressure ulcers. A PIP was put in place with metrics tracking facilty-acquired pressure ulcers and worsening pressure ulcers.
After three-to-four weeks, the facility had zero facility-acquired pressure ulcers, the PIP was made part of standard practice and was transitioned to the care team for ongoing implementation
PIP Communication: Lessons Learned
–Facility And Corporate Communication: Many facilities are owned by larger organizations or corporations, so communication across all entities means sharing information across the enterprise.
–Family Communication: A big part of working with residents means keeping their families informed. Many nursing centers have Family Forums to keep the families engaged.
–Staff Recognition: A big part of any new process is change management. Engaging the staff is critical and recognizing and rewarding desired behavior is a great way to drive change through organizations.