Expense and Staffing Optimization for Senior Care and Living Operators
Pat McCormick, Scott McLellan, and Denise Leonard
3/16/2023
ADVERTORIAL

Nursing homes have been hit the worst of all health care sectors as chronic Medicaid underfunding combined with overwhelming pandemic-related expenses have left them struggling to compete for qualified staff. Since the start of the pandemic, nursing homes have lost 15 percent of their total workforce—more than any other health care setting.
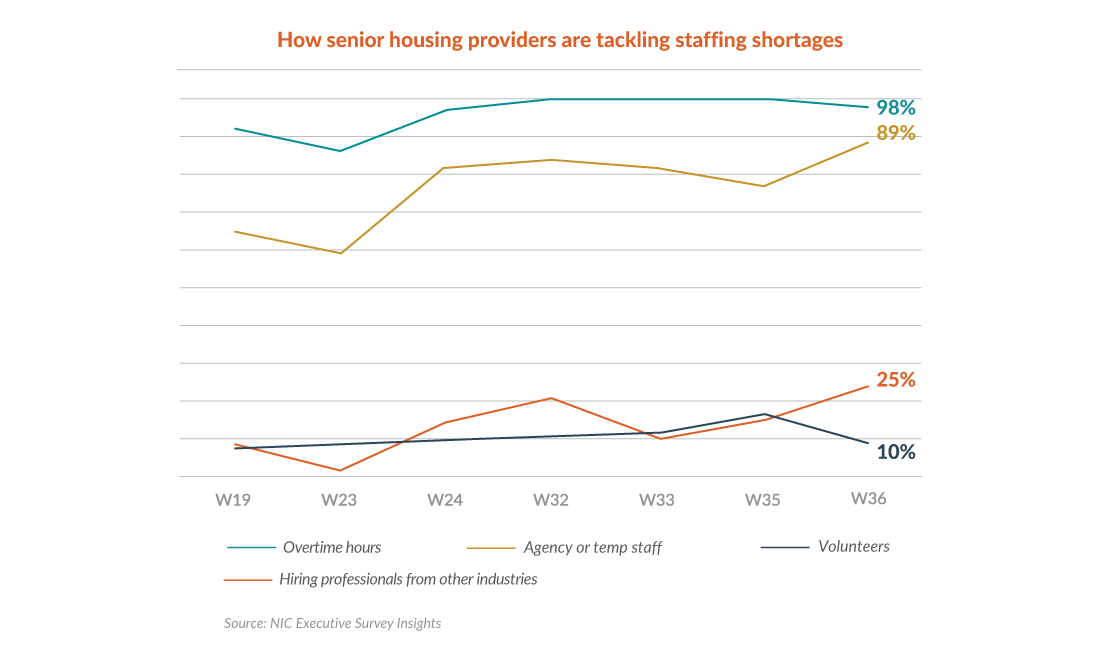
As a result of this severe staffing shortage, providers are almost universally asking employees to work overtime, and the vast majority are backfilling shortages with temporary staffing. A January 2022 NIC Executive Survey showed 98 percent of respondents were paying overtime and 89 percent were using agency or temporary staff. In April 2020, just 85 percent of respondents were paying overtime and 36 percent were using agency or temporary staff.
The growing reliance on temporary staff has driven dramatic increases in agency costs. In hot markets, contract nurses can essentially name their price, particularly with the introduction of online platforms. One example is KARE, a platform that connects senior care and living providers with independent contractors, who set their own pay scale.
Competition for nurses is especially fierce. In 2021, registered nurse salaries increased about 4 percent to $81,376, according to a Wall Street Journal analysis of nearly 60,000 nurse salaries, excluding overtime and bonus pay. In 2020, nurse salaries increased 3.3 percent and in 2019, 2.6 percent.
 Labor and contract disputes in a number of states are contributing to nationwide wage rate increases. In the face of possible strikes, a Connecticut health system settled on a $20-per-hour minimum for certified nursing assistants (CNAs) and $30 per hour for licensed practical nurses (LPNs). A landmark contract case in Oregon resulted in wage increases of as much as 30 percent, pushing minimum rates for CNAs to $18 per hour.
Labor and contract disputes in a number of states are contributing to nationwide wage rate increases. In the face of possible strikes, a Connecticut health system settled on a $20-per-hour minimum for certified nursing assistants (CNAs) and $30 per hour for licensed practical nurses (LPNs). A landmark contract case in Oregon resulted in wage increases of as much as 30 percent, pushing minimum rates for CNAs to $18 per hour.
In addition to competing with deep-pocketed hospitals and health systems—some of which are offering nurses double-digit increases—long term care providers are increasingly seeing caregivers jump ship to join staffing agencies, where they can often earn higher hourly wages while meeting their needs for flexibility.

There have been some innovative approaches to help providers alleviate the staffing crisis, such as a Minnesota initiative to recruit at least 1,000 new CNAs. The American Health Care Association (AHCA) and LeadingAge are advocating for Care for Our Seniors Act, which includes provisions to recruit and retain more long-term caregivers, as well as to enhance quality of care, oversight, and safety of facilities.
But for struggling senior care providers, these reforms could come too late. Most providers are spending government stimulus dollars to cover compensation increases, but given the rigid constraints of Medicaid reimbursement rates, the long-term viability of these higher wage rates remains murky at best. Considering that, pre-pandemic wages and benefits accounted for about two-thirds of the typical senior care provider's cost structure, these sharply increasing labor expenses aren't sustainable without an increase in Medicaid and Medicare reimbursement.

What's Next?
The bottom line is that providers need to step back and look at the business in a methodical way. The senior care landscape has changed significantly, and strategies that weren't possible even five years ago are available and becoming mainstream. For health care leaders, future growth and profitability hinge on new ways of thinking and a shift in perspective to reimagine what's possible.
Patrick McCormick is a partner and practice leader for Plante Moran's capital projects group, specializing in financial and market feasibility studies for senior care and living organizations.
Scott McLellan is a partner and leader for Plante Moran's Group Benefits & Brokerage Services, working with clients to develop cost-effective benefit strategies.
Denise Leonard is a partner, CPA, and leader for Plante Moran's senior care and living reimbursement practice focusing on guiding health care organizations through the ongoing changes in reimbursement and industry issues.