When President Obama pitched his plan for health care reform in June 2009, few health care companies were surprised at his announcement that “almost 20 percent of Medicare patients discharged from hospitals are readmitted within a month.”
What did send ripples through the medical community, however, was Obama’s statement that “changing how Medicare reimburses hospitals…will save us $25 billion over the next decade.”
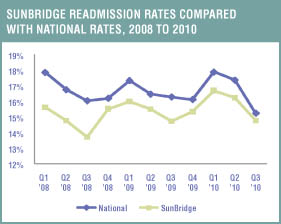
SunBridge Healthcare has taken an active role in partnering with hospitals in various communities around the country to help identify the causes and decrease the percentages of readmissions. According to Sandy Gigandet, SunBridge’s regional director of clinical operations for Indiana and Ohio, “Our goal is to decrease our unplanned discharges back to the hospital to less than 10 percent, realizing that some components are beyond our control.”
In fact, SunBridge has been using a hospital management system for more than four years that allows a review of hospital readmissions by time, date, provider, physician, and diagnosis/symptom and also in relation to admission and payer sources.
This dynamic system allows for a thorough identification of trends at multiple levels, from individual centers to entire divisions. By examining a variety of trends revealed by the data, Jackie Strader, SunBridge’s regional director of clinical operations for Kentucky North, uncovered a variety of related causes.
“If I had to sum up our findings in one word, I’d say education—of our staff, of our attending and on-call physicians, and even of our residents,” Strader says. In some communities where a specific clinical need is identified, SunBridge centers have developed services and supported their staff in receiving the unique training required to sustain these services.
Community Partnerships
At Regis Woods Care and Rehabilitation Center, Louisville, Ky., for instance, the team consulted with staff at Baptist Hospital and learned that area nursing facilities didn’t provide total parenteral nutrition care (TPN). Armed with this knowledge, the clinical team at Regis Woods pursued training regarding appropriate TPN care and equipment. Now the center is able to admit and care for residents with these clinically complex conditions rather than having to discharge them back to the hospital.
Other SunBridge centers are following suit, depending on the particular needs of their communities. Triad Care and Rehabilitation Center of High Point, N.C., is currently developing a stroke recovery unit, while Willows Care and Rehabilitation Center, Woodbridge, Conn., offers services like dialysis management.
Some SunBridge centers are taking a broader approach by partnering with local hospitals to address common diagnoses that frequently result in unplanned discharges.
For example, Marilyn Morel, one of SunBridge’s clinical care specialists in New Hampshire, has been working with staff from Cheshire Medical Center/Dartmouth-Hitchcock Keene for several months to decrease unplanned discharges from nursing centers that result from congestive heart failure (CHF). Together they have created a “discharge order set” that helps increase communication among hospital physicians and nursing center staff.
Morel praises the initiative, saying, “The discharge order set has not only helped with continuity of care but also helped build relationships between the hospital and center staff. That can only benefit the residents.”
Cheshire is not the only hospital partnering with skilled nursing centers. Bedford Hills Care and Rehabilitation Center, in Bedford, N.H., for example, has adopted clinical CHF protocols. From hospital to nursing facility, these new protocols help ensure a continuity of care that benefits patients and lowers the number of readmits to the hospital, especially in the 30-day window after discharge.
Since the protocols were implemented in February 2010, both Bedford Hills and Elliot Health System have been pleased to see the hospital readmission rate decrease to a mere 12 percent. “I view this move toward collaboration and accountability as a positive advancement, both for the staff and also for the patients,” says Malcolm Perry, director of Senior Health Services for Elliot Health System.
Recognizing Changes
One critical factor in decreasing unplanned discharges is early recognition of a change in condition in a resident. Part of SunBridge’s procedures includes a Change in Condition form, a tangible, useful tool that assists clinical staff in pulling together resident information such as vitals, general appearance, physical evaluation, recent lab results, and medications on a one-page reference sheet.
In fact, centers are so adamant about recognizing a change in a resident’s condition that all clinical staff undergo training on this topic first during their initial orientation and then annually thereafter. Furthermore, staff development personnel at each center complete annual competency reports for all members of the clinical staff to help ensure that competencies in key skilled areas are being met.

A very practical approach to care is implemented on a daily basis in SunBridge centers. Certified nurse assistants are trained to record their observations during every shift on a Nursing Assistant Worksheet and to report any changes in a resident’s condition to the licensed nurse on duty. The licensed nurse then completes an assessment using the Change of Condition form and also documents any changes on a 24-hour report sheet.
In addition, the licensed nurse notifies the resident’s physician, making sure to document any new orders, and also notifies the resident’s family. After the new orders are implemented, the resident is monitored for improvement on each shift with oversight by the center’s director of nursing.
Center administrators also play a role in helping to reduce hospital readmissions by reviewing their “top five” at-risk residents every morning in a stand-up meeting with their interdisciplinary teams. In addition, clinical staff review what’s known as the Radar Report, a minimum data set-based report that assists centers in identifying residents at risk as well as residents who have been evaluated to have a change in condition.
This approach helps provide early identification of potential concerns, resulting in the opportunity for early intervention, staff education, and improved clinical outcomes.
As hospitals have discharged their patients “quicker and sicker,” skilled nursing facilities have had to increase their abilities to care for these higher-acuity patients. “One way we’ve addressed that challenge,” Strader says, “beyond providing increased training for our existing staff, is to hire more registered nurses [RNs]. In SunBridge’s Kentucky North region, for example, we’ve increased the number of RN staffing positions by 17 percent in 12 months. During that same time frame, we have seen a decrease in unplanned discharges.”
Bridge Point Care and Rehabilitation Center in Florence, Ky., reduced its unplanned discharges per month approximately 31 percent from the fourth quarter of 2009 to the first quarter of 2010. Not only did they focus on staff education but they also hired six additional RNs last year.
Gigandet adds, “Each of our centers strives to have a nurse practitioner or physician’s assistant on board in addition to a medical director. Whenever possible, we prefer our physicians also practice a specialty at our referring hospitals to help ensure continuity of care upon admission into our centers. This approach allows us to continue the same protocols initiated in the hospital.”
Promoting Physician Awareness
Susan Coppola, SunBridge’s senior vice president of clinical operations, points out that it is often to the resident’s medical advantage to remain in the center rather than return to the hospital. “Our goal is to achieve continuity and meet our residents’ needs whenever possible while keeping them in place,” Coppola says.
If this is true, then why do some physicians discharge their residents back to the hospital? In reviewing the data, Strader discovered that some of SunBridge’s unplanned discharges occurred because attending and on-call physicians were unaware of the centers’ capabilities.
“We had to educate them as to our ability to provide stat labs, various diagnostic procedures, and specific medications from our pharmacies. Once they realized that we could provide these and other services, they were less anxious to readmit their residents to the hospital for the same services,” Strader says.
The Patient’s Role
Yet another reason for hospital readmissions, especially within 30 days of discharge, is a lack of patient compliance by individuals who return directly home. In other words, patients are discharged from the hospital without any post-acute services, they do not see their primary care physicians within 30 days of being discharged, or they refuse to follow the diet and exercise protocols as established as part of their discharge instructions.
SunBridge facilities are trying to address some of these factors by partnering with local hospitals to position the facilities as a viable post-acute services alliance that can help decrease preventable readmissions. Upon admission to a center, for instance, the resident and his or her family members are invited to a Customer First Post-admission Conference.
“This conference is important not only for developing an appropriate plan of care,” says Coppola, “but also for establishing realistic expectations and for helping the resident and family understand the services we provide.”
Having such a meeting creates a level of confidence in the resident and family so that, should a change in condition occur, the resident and family understand that a return to the hospital is not necessarily the first step in the process, Coppola says.
Coleen Maddy is the publications editor for Sun Healthcare Group. She can be reached at coleen.maddy@sunh.com or (505) 468-6864.