PDPM Data Trends Part III: PDPM Isolation Policy Hurt Providers that Followed Public Health Guidance
Daniel Ciolek
6/1/2022
This is the third of a series of articles related to the implementation of the Patient-Driven Payment Model (PDPM) supported by examples of data trends reported by the Centers for Medicare & Medicaid Services (CMS), academic researchers, as well as analyses conducted by AHCA/NCAL. The series will delve into questions related to patient care delivery, outcomes, and payment model implications informed by observed PDPM data trends.
In the Fiscal Year (FY) 2023 Skilled Nursing Facility Prospective Payment System (SNF PPS) proposed rule1, CMS issued a Request for Information (RFI) on whether PDPM adequately accounts for patient care needs associated with an active infectious disease requiring quarantine. Here AHCA/NCAL presents evidence suggesting that CMS should modify their isolation policy to mitigate for significant PDPM rate disparities when following CMS and Centers for Disease Control (CDC) public health guidance to cohort such patients during public health emergencies (PHE).
Historically, SNF patients that require isolation and treatment for “highly transmissible or epidemiologically significant pathogens that have been acquired by physical contact or airborne or droplet transmission” have been classified into one of the highest intensity Nursing component extensive services case-mix groups based on time study analyses. The SNF Minimum Data Set Resident Assessment Instrument (MDS-RAI) directs that SNFs may only code MDS item O0100M2 – Isolation or Quarantine for Active Infectious Disease if a resident requires transmission-based precautions, is placed in single room isolation, and remains in the room2. Under PDPM, Medicare patients with the MDS isolation or quarantine item reported are classified into the ES1 Nursing component case-mix group (CMG). This isolation item is also assigned one non therapy ancillary (NTA) component point, which could elevate patients into the next higher NTA CMG.
During the COVID-19 PHE, with massive numbers of quickly spreading cases overwhelming hospitals and SNFs, CMS recognized there was an insufficient capacity of single-occupancy isolation rooms and issued blanket waivers effective March 1, 2020, permitting “grouping or cohorting residents with respiratory illness symptoms and/or residents with a confirmed diagnosis of COVID-19, and separating them from residents who are asymptomatic or tested negative for COVID-193.” The waiver further specified that cohorting residents “aligns with CDC guidance to preferably place residents in locations designed to care for COVID-19 residents, to prevent the transmission of COVID-19 to other residents.”
From January 2020 through September 2021 there were 521,570 SNF PPS MDS assessments containing a diagnosis code of an active COVID-19 infection, with 80.9 percent of patients located in urban counties. During this time span, only 44.9 percent of patients with an active COVID-19 infection were able to be isolated into a single-occupancy room. The remaining 287,379 beneficiaries were in cohorted quarantine following CMS guidelines and therefore were ineligible for the Nursing component ES1 classification or the additional NTA point. Both components defaulted to lower valued CMGs as if the patient’s active COVID-19 condition requiring significant care needs did not exist.
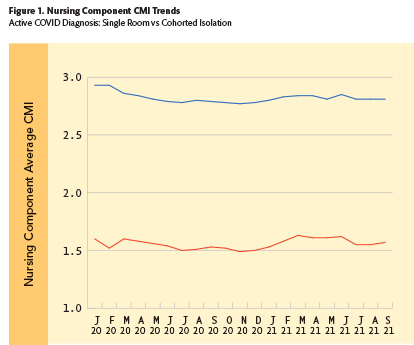
The devastating impact of this policy shortfall is reflected in Figure 1 that depicts the monthly average Nursing component CMIs for SNF Medicare patients in urban locations with an active COVID-19 diagnosis. The blue line shows that patients in single room isolation had nursing component CMIs nearly double those of patients in cohorted room isolation (red line).
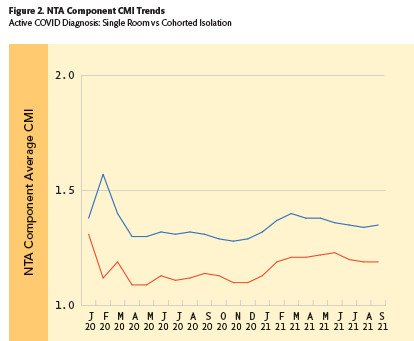
In a similar but less dramatic manner, Figure 2 depicts the monthly average NTA component CMIs for SNF Medicare patients in urban locations with an active COVID-19 diagnosis. Here, the blue line shows that patients in single room isolation had NTA component CMIs which were about 15 percent higher than those of patients in cohorted room isolation (red line).
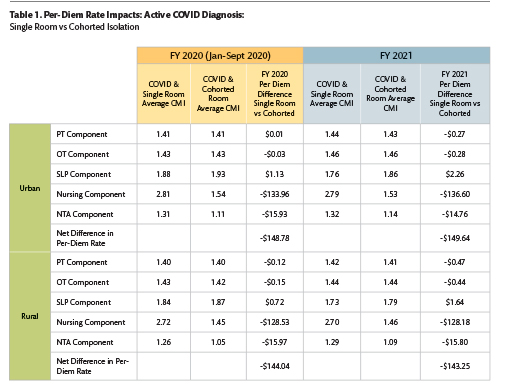
The impacts on total PDPM per-diem rates were substantial. Table 1 includes the average CMI and federal per-diem rate impacts for each PDPM component observed for all patients with an active COVID-19 diagnosis, comparing patients in single room versus cohorted room isolation during both FY 2020 and FY 2021. It is striking that while there were nominal differences in CMIs and payments for the PT, OT, and SLP components for COVID patients across all variables, there were substantial differences in the Nursing and NTA components. As depicted by the cells with bold text, the net daily reimbursement difference for cohorted COVID-19 patients was nearly $150 per day in urban and rural locations across both years, driven by significant CMI inequities in the Nursing and NTA components for active COVID patients that were placed in cohorted quarantine.
AHCA/NCAL believes that there are no differences in the care needs of Medicare beneficiaries with an active COVID-19 or similar highly transmissible infection that justify maintaining an arbitrary and inflexible isolation coding policy that penalizes providers for following public health guidance. AHCA/NCAL is submitting comments to CMS requesting the Agency revise the definition of MDS Item O0100M2 to create a pathway for coding cohorted isolation when the provider is following government infection control guidance, and that the PDPM payment model is revised to remove the unfair payment discrepancies described here.
Readers may submit comments to CMS about the FY 2023 SNF PPS proposed rule through AHCA/NCALs Voter Voice at: https://www.votervoice.net/AHCA/Campaigns/93978/Respond. Comments must be submitted by June 10, 2022.
Daniel Ciolek is associate vice president, Therapy Advocacy, for the American Health Care Association.
1 �87 FR 22720. April 15, 2022. Medicare Program; Prospective Payment System and Consolidated Billing for Skilled Nursing Facilities; Updates to the Quality Reporting Program and Value-Based Purchasing Program for Federal Fiscal Year 2023; Request for Information on Revising the Requirements for Long-Term Care Facilities To Establish Mandatory Minimum Staffing Levels. CMS-1765-P
² CMS MDS RAI Manual, Version 1.17.1., October 2019
³ �COVID-19 Emergency Declaration Blanket Waivers for Health Care Providers