
When Rosie Connectivity Solutions and Xandar Kardian (XK) announced their partnership in January 2025, no one could have predicted how personal that collaboration would become.
Months later, Rod M., a respected leader at Rosie who had dedicated his career to technologies that supported caregivers and improved patient care, received a devastating diagnosis: advanced pancreatic cancer. As the end approached, Rod made an extraordinary request to be monitored by XK's contactless radar sensor during his final two weeks at home.
Not for treatment, but for insight. So that others walking the same path might have more clarity, more time, more dignity.
"Rod's story stands as a testament to the integrity of his vision," says Brittany Jefferson, Chief Commercial Officer at Rosie. "In his final days, the Xandar Kardian sensor provided the very information and support he had long advocated for."
The Ambient Health Monitor

A small sensor sat on Rod's bedside table like a lamp, using contactless radar to capture his vital signs without ever touching him. No wires, no wearables, no cameras. It simply monitored, capturing over 8,000 heart rate and 10,000 respiratory rate measurements each day.
What it captured told a story that human observation alone couldn't have.
What Rod's Body Was Telling Us

The First Week
For the first week, Rod's vital signs remained stable, with Respiratory rate around 16 breaths per minute and heart rate near 73. He spent time with family and slept normal hours.
Six Days Before: When Everything Changed
Rod's sleep extended to over 20 hours daily. His movement declined until he became almost motionless.
His respiratory rate dropped from 16 to 9 breaths per minute, falling below the normal range and never recovering. More revealing was how his breathing lost its natural variability i.e. the ability to adapt to changing needs. The sensor captured the actual shape of each breath: waveforms showing pauses stretching to 8 seconds, inhalations becoming progressively longer, a pattern that had lost its rhythm. Estimated airflow fell by nearly 50%.
His heart rate rose from 73 to 87 beats per minute. Both numbers fall within "normal" range - a nurse checking his pulse would have recorded acceptable values. But continuous monitoring revealed a significant deviation from Rod's baseline. His heart rate lost its variability, beating at a steady, elevated pace regardless of rest or activity.
The Pulse-Respiration Quotient [heartbeats per breath] rose from the normal range of 3-6 to 10. His heart was racing while his breathing slowed, signaling growing physiological strain.

Continuous monitoring revealed patterns invisible to traditional spot checks
The Window We Never Had Before
All of these changes began six days before Rod passed. Not in the final hours. Six days before, when there was still time to gather, to prepare, to comfort.
Traditional spot checks would have missed these signals entirely. Individual readings were normal. It was the pattern, the deviation from Rod's own baseline, that told the story.
Beyond One Journey
Rod's family and the teams at Rosie and XK asked: Was this pattern unique to Rod, or universal?
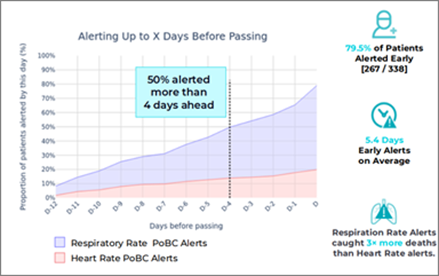
Analysis of 338 patients in Long Term Care confirmed what Rod's journey suggested: Nearly 80% showed detectable vital sign changes before death, appearing an average of more than five days in advance.
"What we discovered goes beyond technology," says Sam Yang, CEO of Xandar Kardian Inc. "These patterns reveal a window of time, often five or more days, where families can gather, clinicians can adjust care, and providers can allocate resources with confidence. That window changes everything."
What Five Days Means![]()

Five days create time for what matters most - Presence, Comfort, and Closure
Five days is the difference between a daughter arriving in time to hold her father's hand or arriving to an empty room. It's the space for final words spoken to a living person, not a gravestone.
But that window of time creates measurable impact across the organization:
For Families:
- Time to gather loved ones from across the country
- Opportunity for meaningful closure and final conversations
- Preparation instead of shock
For Clinical Teams:
- Proactive symptom management before discomfort intensifies
- Confident conversations with families about what to expect
- Shift from crisis-driven care to planned comfort measures
For Provider Operations:
- Continuous monitoring reduces the burden of frequent manual vital sign checks, allowing nursing staff to focus on direct patient care and family support
- Early detection supports the strategic allocation of nursing resources to patients with the greatest need, with a detection rate of 79.5%
- 5+ days advance notice helps prevent the crisis-driven situations that are stressful for both staff and families
Monitoring Reimagined
Contactless monitoring isn't there to trigger treatments or suggest intervention. It's there to capture what the human eye cannot see, to reveal patterns that help everyone respond with compassion.
This is monitoring in service of comfort, not intervention. Awareness in service of dignity.
Honoring the Gift
"Rod wanted his experience to ease the path for those who follow," Jefferson reflects. "Through his generosity, patterns once invisible have become measurable. Changes once noticed too late can now be recognized days in advance."
Rod believed technology could make care more compassionate and human. In his final act, he proved it. His legacy lives on in what that enables: families who get to say goodbye, caregivers who provide comfort at exactly the right moment, and patients whose final days are marked by peace rather than crisis.
The complete whitepaper includes detailed waveform patterns, day-by-day progression data, and comprehensive analysis across 338 patients. The Findings go far beyond what we can share here.
Click here to download "Continuous Health Monitoring in End-of-Life Care" whitepaper.
The XK300-H sensor used for the study is an FDA-cleared, contactless monitoring device recognized as a TIME Best Invention 2024 and CES Innovation Award winner.