PDPM Data Trends Part IV
Unresolved COVID “Spillover Effects” in CMS Proposed PDPM Parity Adjustment Approach
Daniel Ciolek
8/9/2022
This is the fourth of a series of articles related to the implementation of Patient-Driven Payment Model (PDPM) supported by examples of data trends reported by Centers for Medicare & Medicaid Services (CMS), academic researchers, as well as analyses conducted by AHCA/NCAL. In this series we will contemplate questions related to patient care delivery, outcomes, and payment model implications informed by observed PDPM data trends. For previous articles, visit providermagazine.com.
On October 1, 2019, CMS implemented the new skilled nursing facility prospective payment system (SNF PPS) case-mix index (CMI) classification model called the Patient-Driven Payment Model (PDPM). CMS intended for PDPM to be budget neutral, meaning that the new payment model would not result in an increase or decrease in aggregate SNF spending.
In the fiscal year (FY) 2023 SNF PPS proposed rule1, CMS discussed the lengths taken to address concerns raised in last year’s proposed approach to account for the impact of COVID-19 public health emergency (PHE) on costs and data trends. CMS proposed a modified “Control-Period-based Adjustment Factor” using data from the six months in FY 2020, before the first major COVID wave, and the last 6 months of FY 2021, where COVID was the least prevalent. After applying the new approach, CMS continues to note higher than expected PDPM spending, and proposed a parity adjustment of 4.6 percent (which is lower than the 5.0 percent proposed last year).
AHCA appreciates the deliberative approach the Agency has taken to date to mitigate for the impacts of the COVID-19 PHE on PDPM payments to best assure that any finalized parity adjustment determination does not result in an overcorrection that could negatively impact beneficiary access to care. We note that the Agency followed through with addressing many of the questions AHCA raised in response to last year’s proposed rule related to COVID “spillover” effects on the parity adjustment analysis data. While we believe this year’s proposal is an improved approach, we continue to believe that there is COVID “spillover” that has yet to be accounted for.
“Spillover” occurs in non-COVID patient CMIs when minimum data set (MDS) patient assessment item patterns change from what would have occurred if not for the pandemic. In this article we share two examples of MDS data patterns for patient pressure ulcers and non-COVID related respiratory failure characteristics that reflect increased care needs at levels not observed prior to the COVID-19 PHE that remained elevated even during the low-COVID months. In submitted comments to CMS, AHCA concluded that these and other trends suggest unresolved “spillover” that, if accounted for, would reduce the parity adjustment lower than the amount proposed2.
MDS Pressure Ulcers and Injuries
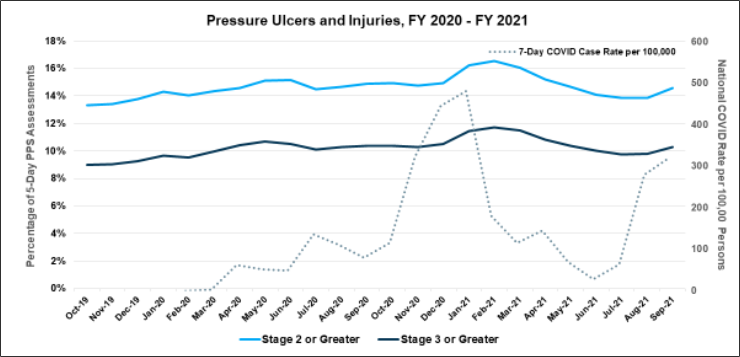
The SNF PPS 5-day MDS assessment item trends during the PHE in non-COVID Part A admissions related to pressure ulcers shifted (Figure 1). Specifically, the presence of Stage 2 Pressure Ulcers or greater (Items M0300B1-G1), depicted by the light blue line, and Stage 3 Pressure Ulcers or greater (Items M0300C1-G1), depicted by the dark blue line increased during the initial and subsequent COVID surges (dotted grey line), and remained elevated above pre-COVID levels, even during low COVID months in FY 2021. Because these wounds were present upon the Part A Admission, they do not reflect wounds incurred during the Part A stay but do reflect higher acuity needs upon admission than was present pre-PHE. Because such wounds typically require specific time-intensive nursing treatments, these patients typically are classified into the higher acuity PDPM Nursing component Special Care Low case -mix group (CMG). In addition, Stage 4 pressure ulcers (Item M0300D1) are assigned one NTA component point which could elevate the CMG assigned for that component. As such, AHCA believes the currently proposed parity adjustment approach will not adequately mitigate for the observed shift in reported pressure ulcer conditions of non-COVID patients upon Part A admission that were elevated throughout the PHE, including low COVID months.
Figure 1. The Percent of Patients with Pressure Ulcers in Non-COVID Part A Admissions Spiked During COVID Surges and Remained Elevated Above Pre-PHE Levels
MDS Respiratory Failure
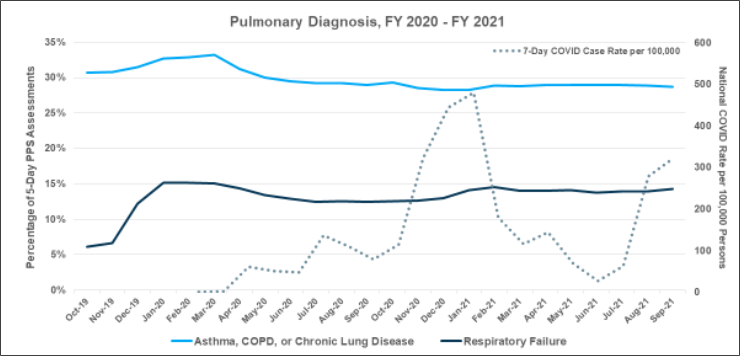
Other SNF PPS 5-day MDS assessment item trends during the PHE in non-COVID Part A admissions such as item I6300 - Respiratory Failure conditions also spiked at the onset of the PHE and remained elevated throughout the PHE (dark blue line in Figure 2). While these patients did not have a COVID diagnosis when the 5-day assessment was performed, the proportion of SNF stays involving such patients with respiratory failure for other reasons has shifted from approximately 6 percent prior to the COVID-19 PHE to about 14 percent throughout the PHE. Such a shift results in “spillover” effects on the parity adjustment analysis even during low COVID months as it reflects an increase in the SNF patient population acuity compared to the pre-COVID months.
When such patients require oxygen therapy, they are classified into one of the higher PDPM Nursing component Special Care Low CMG groups. Again, AHCA believes the currently proposed parity adjustment approach will not mitigate for the observed shift in reported respiratory conditions of non-COVID patients that did not follow COVID surge patterns, and therefore reflects a higher patient acuity patient upon admission than was present pre-PHE, even in low COVID months.
Figure 2. Share of Non-COVID Respiratory Failure Admissions Spiked Throughout the PHE
The CMS Decision
Prior to publication of this article, CMS published the FY 2023 SNF PPS Final Rule3 in which CMS decided to adopt the proposed 4.6 percent parity adjustment to mitigate for the COVID “spillover” effects to be applied to future SNF payments. The final rule that applies to Medicare Part A SNF payment rates effective October 1 will be phased in at 2.3 percent in FY 2023 and an additional 2.3 percent in FY 2024. AHCA intends to continue to monitor these trends to inform future rulemaking advocacy.
Daniel Ciolek is associate vice president, therapy advocacy, for the American Health Care Association.
References
1. 87 FR 22720. April 15, 2022. Medicare Program; Prospective Payment System and Consolidated Billing for Skilled Nursing Facilities; Updates to the Quality Reporting Program and Value-Based Purchasing Program for Federal Fiscal Year 2023; Request for Information on Revising the Requirements for Long-Term Care Facilities to Establish Mandatory Minimum Staffing Levels. CMS-1765-P (https://www.federalregister.gov/documents/2022/04/15/2022-07906/medicare-program-prospective-payment-system-and-consolidated-billing-for-skilled-nursing-facilities)
2. AHCA FY23 SNF PPS Final Comment Letter. June 3, 2022. Comment ID CMS-2022-0069-2654. (https://www.regulations.gov/comment/CMS-2022-0069-2654)
3. 87 FR 47502. August 3, 2022. Medicare Program; Prospective Payment System and Consolidated Billing for Skilled Nursing Facilities; Updates to the Quality Reporting Program and Value-Based Purchasing Program for Federal Fiscal Year 2023; Changes to the Requirements for the Director of Food and Nutrition Services and Physical Environment Requirements in Long-Term Care Facilities. CMS-1765-F (https://www.govinfo.gov/content/pkg/FR-2022-08-03/pdf/2022-16457.pdf)