SNFs Break The Infection Chain
Disinfecting medical equipment and environmental surfaces is vital to stopping the spread of harmful microorganisms.
J. Hudson Garrett, Jr., PhD
3/1/2010
Now, more than ever, disinfection of the resident’s environment is a key component of the infection prevention and control process in the long term care setting. One of the most critical interventions that can be routinely performed to decrease the risk for cross transmission and development of health care-associated infection is routine cleaning and disinfection of the health care environment.
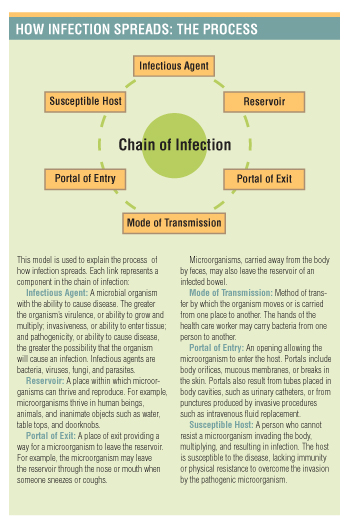
Cross contamination can occur in a variety of ways, but an environmental surface often becomes contaminated and then serves as a reservoir for microbial growth. The hands of either the health care provider or the patient come in contact with this contaminated surface, and contact is made with another device or surface, thereby contaminating it as well. Thus the chain of infection transmission begins.
Clean Surfaces First
The ability of microorganisms to successfully survive and reproduce on environmental surfaces has never been greater. Organisms such as Methicillin-resistant Staphylococcus aureus, Escherichia coli, Clostridium difficile (C-diff.), and Mycobacterium tuberculosis can survive on surfaces for several months. C-diff. and other organisms, such as Vancomycin-resistant Enterococci, continue to plague the long term care environment. Because of the resilience of these microorganisms, it is important to routinely disinfect potentially contaminated surfaces to reduce the risk of transmission.
Before effective disinfection can occur, it is important to thoroughly clean visibly soiled environmental surfaces to allow for the full efficacy of the chosen disinfectant product. Cleaning—as defined by the latest Centers for Disease Control and Prevention (CDC) Guideline for Disinfection and Sterilization in Healthcare Facilities, released in 2008—is “the removal of foreign material, such as soil, and organic matter, from objects, and is normally accomplished using water with detergents or enzymatic products.”
CDC also emphasizes that thorough cleaning is essential before conducting high-level disinfection and sterilization “because inorganic and organic materials that remain on the surfaces of instruments interfere with the effectiveness of these processes.”
Cleaning removes bioburden—the number of bacteria living on a surface before it is sterilized—from the affected surface by reducing the number of microorganisms that must be inactivated. Removing bioburden from the surface prior to application of the disinfectant will result in increased disinfectant efficiency.
It is also important to apply friction to the area being cleaned and disinfected in order to remove more resistant forms of microorganisms such as spores and C-diff. from the surfaces that may not be readily inactivated by the disinfectant. This will decrease the risk for development of multidrug-resistant organisms.
High-touch surfaces such as blood pressure cuffs, stethoscopes, and glucometers require frequent disinfection to prevent cross-transmission between residents. The physical number of microorganisms present on any given surface is influenced by a number of factors, including the amount of moisture present on the surface, the amount of activity taking place in the immediate environment, the number of people having contact with the environment, and the type of environmental surfaces present and their ability to support the growth of microorganisms.
Critical And Noncritical Items
The primary focus of a thorough environmental disinfection program should be on those items that are used with multiple residents and/or procedures. E.H. Spaulding created a standardized approach to disinfection in the health care environment that consists of three categories: critical, semi-critical, and noncritical.
- Critical items are those that will enter sterile tissue or the vascular system or areas in which blood flows would be sterile. The objective with disinfection of these items is complete sterility, which can be achieved through a variety of techniques such as ethylene oxide sterilization, gas hydrogen, chemical, or steam sterilization. Examples of critical items include intravenous catheters, implant devices, needles, urinary catheters, cardiac monitoring catheters, and surgical instruments.
- Semi-critical items are those that will come in contact with mucous membranes and/or intact skin. The objective for disinfection with these items is to eliminate all vegetative microorganisms, including viruses, bacteria, fungi, and mycobacteria. These items require high-level disinfection through use of chemical disinfectants.
- The most frequently used items in the long term care facility are noncritical items, such as wheelchairs and bedside tables, because they have contact with intact skin, but not sterile body tissues or mucous membranes. These items require the use of a low-level disinfectant. With the recent migration of electronic medical records in many acute care facilities, disinfection of noncritical items such as computer keyboards is important to reduce transmission of microorganisms throughout the entire environment. Hand hygiene in these circumstances is still the most critical intervention to break the chain of infection, but routine disinfection of these potential reservoirs for microbial growth is also a key component. It is critical to have a complete set of policies and procedures identifying each individual’s and department’s responsibility in the cleaning and disinfection process. Careful collaboration with the environmental services team is necessary in order to ensure that all surfaces are routinely disinfected by the appropriate personnel. Educational programs are available through organizations such as the Association for Professionals in Infection Control and Epidemiology (APIC) or the American Society for Healthcare Environmental Services. Involvement of all staff members, including executive management and nurse leaders, is critical to the success of an environmental disinfection program.
Waiting Room Breeds Bacteria
Educating health care staff is key to minimizing risks associated with using any disinfectant product. Staff members should be trained on the appropriate indications for use of the product; the instructions for use, including total overall contact time required to effectively inactivate the microorganisms on the product’s efficacy label, known as the material safety data sheet; and the appropriate use of personal protective equipment as required by the Occupational Safety and Health Administration’s Bloodborne Pathogens Standard.
Training on the appropriate use of the chosen product will ensure the product’s effectiveness and protect end users from adverse reactions.
The waiting room of any a long term care facility is an excellent place for bacteria to breed due to the high-traffic nature of these unique environments. Residents also frequent these locations to visit with other residents, family members, and visitors. This creates an opportunity for transmission of infection between the resident and visitor, as well as between any environmental surfaces.
One of the most efficient and economical ways to prevent infection transmission is to provide visitors and residents hand hygiene products for use immediately upon entering the facility. This simple intervention will prevent most microbes from entering the facility and being transmitted to residents and staff. It is also critical to properly educate visitors entering the facility about infection prevention standards for hand hygiene and isolation to ensure compliance with all current policies and procedures.
Environmental services staff should thoroughly disinfect the waiting room and all items within each and every day with a facility-approved disinfectant to prevent microbial growth as a result of contamination.
It is critical to involve all parties, including residents as well as visitors, in the infection prevention process to ensure success. A thorough cleaning and disinfection program combined with careful selection of the most appropriate hospital-grade disinfectant will dramatically improve the daily fight against health-care-associated infections.
For More Information
- APIC and Professional Disposables International have created a toolkit for educating health care facilities on proper infection prevention techniques and solutions. To request a free copy, which includes a facilitators guide; motivational posters in English and Spanish; case studies on hand hygiene, surface disinfection, and skin antisepsis; a resource guide; and a motivational video, go to: ww.pdipdi.com/champions_kit.aspx.
J. Hudson Garrett Jr., PhD, is director of clinical affairs at Professional Disposables International, Orangeburg, N.Y. He can be reached at hgarrett@pdipdi.com.