An East Coast skilled nursing facility (SNF) administrator had a very efficient secretary. She sorted his mail and threw away everything that looked like junk. This worked well until a nondescript white envelope from TMF Health Quality Institute arrived in the mail. The efficient secretary threw it in the circular file.
The envelope contained sensitive data about the facility’s Medicare performance via an initiative known as Program for Evaluating Payment Patterns Electronic Report (PEPPER).
It’s Not Junk Mail
TMF is the contractor for the Centers for Medicare & Medicaid Services (CMS) PEPPER program. It is tasked with preparing a report for each SNF that identifies areas of potential improper payments.
Using UB-04 billing claim data provided by the facility’s Medicare Administrative Contractor (MAC), the report contains tables, graphs, and details about specific target areas known to be at high risk for billing errors.
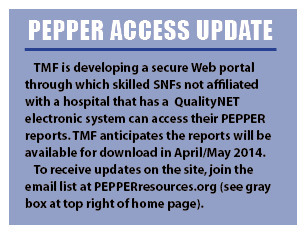
While SNFs that are part of a hospital system have access to PEPPER through the acute care hospital’s QualityNET electronic system, other SNFs will receive their PEPPER report in the mail, addressed to the facility’s chief executive officer/administrator.
According to TMF, the next official SNF PEPPER reports will be available in May 2014. The next round of reports will cover claims data for Medicare “episodes of care” that ended during the federal fiscal years (Oct. 31 through Sept. 30)of 2011, 2012, and 2013.
Areas Of Concern
The episode of care is determined by pulling a series of claims for a Medicare A beneficiary, from the earliest to the latest submitted claim. If the last submitted claim indicates that the resident was discharged from Medicare and did not return for continued care for at least 30 days, that episode of care will be included in the report year in which the last claim “through” date falls.
The PEPPER report focuses on six CMS-targeted areas that use the Resource Utilization Groups (RUGs), which classify patients into case-mix-driven payment categories and have a high likelihood for improper payments.
These target areas include the following:
■ Therapy RUGs with a high score for activities of daily living (ADLs), indicating that a facility may be reporting more assistance than was actually needed (up-coding), resulting in overpayment.
■ Non-therapy RUGs with high ADLs, indicating a potential for up-coding, resulting in overpayment.
■ Change-of-therapy (COT) assessments, which are required when the amount of therapy provided no longer reflects the RUG level.
According to the TMF Skilled Nursing Facility PEPPER Training, Session 1, “SNFs that have a high proportion of change-of-therapy assessments may want to investigate whether there are barriers preventing the provision of anticipated services for beneficiaries, care planning, or other issues” (PEPPER, 2014b). Conversely, a facility that has a low proportion of COTs, or none at all, may be targeted by MACs or RACs (Recovery Audit Contractors) for review.
■ Ultra therapy RUGs. This item calculates the proportion of days billed for all therapy RUGs that fell into the Ultra High levels. Facilities with a high percentile ranking of Ultra therapy RUGs, such as RUX, RUL, RUC, RUB, and RUA, are at increased risk for MAC and RAC payment reviews. Facility leaders should ask themselves whether the therapy provided at these levels was “reasonable and necessary.” Using a triple-check process, they should review whether the Minimum Data Set coding is supported by the medical record documentation.
■ Therapy RUGs. This item calculates the proportion of days billed for all therapy RUGs. High levels of therapy RUGs may indicate inappropriate therapy programming. Review coverage decisions by facility nursing and therapy staff to ensure that the care was “reasonable and necessary.”
■ Episodes of care of 90+ days. This target area identifies the proportion of all episodes of care that had a length of stay of 90 or more days. TMF explains that “SNFs that have a high proportion of episodes of care with 90 or more days should ensure that beneficiaries are receiving services that are necessary, and the SNF should also ensure that beneficiaries received skilled care the entire duration of their SNF stay” (PEPPER, 2014b).
Percentages Determine Risk
Each of the six target areas is reported as a percentage ratio of the defined numerator divided by the denominator, multiplied by 100. The SNF’s percentages are then ranked against those of other facilities in the state, within the MAC jurisdiction, and nationally.
Nursing home managers should review their facility rankings as calculated in each of the three comparison
groups.
PEPPER scores above the 80th percentile indicate a potential risk in payment error and should be the focus of internal audit and review activities.
Falling below the 20th percentile ranking for low ADLs or COTs is also an indication for internal quality review.
TMF emphasizes that the PEPPER report is not intended to identify the actual or confirmed presence of improper payments.
“Those can only be confirmed through a review of the medical record, but PEPPER can help give you clues as to where your billing patterns differ from others so that you can take the first step in determining whether issues exist.”
Providers can utilize PEPPER as a resource and launching pad to comply with the 2010 Affordable Care Act requirements for a corporate compliance program. The report results can direct the facility staff audit and quality improvement activities and lead to detecting errors and system problems.
For more information on PEPPER, see TMF Health Quality Institute, 2013.
Be on the lookout for the facility’s PEPPER report this May. And don’t let it end up in the waste basket.
Judi Kulus, NHA, RN, MAT, C-NE, RAC-MT, is vice president of curriculum development for the American Association of Nurse Assessment Coordination. She can be reached at (800) 768-1880.