
Nursing, rehabilitation, and post-acute care providers today are more focused than ever on tracking and improving every aspect of their businesses—from the quality of individualized care to cost management—especially as the Quality Assurance and Performance Improvement (QAPI) initiative continues to develop.
QAPI aims to make nursing homes more accountable by penalizing those that do not meet federal standards. In order to set in place the building blocks to ensure QAPI compliance, providers should take the following first two steps: Build a governing body, and develop a strong team.
Move From Reactive To Proactive
It is of the highest importance to select not only a strong facility-level team that can generate proactive solutions for care, but to have a dedicated governing body that embraces a culture change within a community to bring QAPI to the forefront of care.
This companywide support will help shift the culture of health care from reactive to proactive, bringing the right expertise of each care staff member to the table for the best outcomes and avoiding a key problem that many face: quality communications across every aspect of the
business.
Despite continued improvements in communication in the health care world, specifically with the advancement of electronic medical records (EMRs), care staff often focus solely on their respective disciplines, holding back vital information that could lead to better outcomes and care. If they were to share their data and care plans with one another, each staff member could help support the individual goals created for every resident in order to achieve the highest level of function.
This is where QAPI could be a successful tool for bringing the best of each care provider to the table, with the focus always on individualized care for the resident.
Team Building
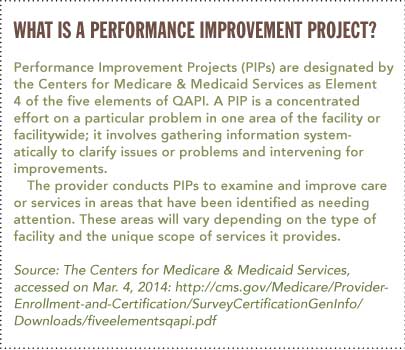
QAPI’s Performance Improvement Projects (PIPs), which implement proactive care initiatives, are only as good as the teams that work on them (see box). When developing a successful PIP, providers first must start with a strong root-cause analysis.
The key here is to bring the team together to discuss the insights and data collection they do on a daily basis. The governing body can design the framework of the PIP and have the necessary tools available to facilitate a productive, objective conversation on improving outcomes while decreasing overall health care costs.
The next step is to bring the experienced caregivers and their objective data to the table. It is important to select the right variety of team members for each specific PIP, and this can include consultants and representatives from outside agencies that support the residents and community.
A Case In Point
Take the discussion of continence care and incontinence product selection for a resident as an example: These topics are extremely important, as they have a direct impact on a resident’s dignity and a potential for risk for slips and falls, infections, and rehospitalizations.
However, they can also bring many challenges, such as the difficulty of discussing the associated cost. In fact, incontinence care as a whole can account for up to 15 percent of a facility’s total costs.
This is where having experienced health care professionals—such as nurses and physical and occupational therapists—present can be incredibly helpful.
Those professionals can help break down stigmas and focus on the data that will lead to better resident outcomes, making the conversation as productive as possible.
Additionally, including consultants and representatives from outside agencies that support the overall community can improve the focus on the resident by explaining all aspects of incontinence products and care practices, possibly uncovering areas of data collection and input from nonclinical staff.
Such areas could include housekeeping, maintenance, central supply, and laundry, all of which are related to incontinence product selection.
Together, the community staff and external representatives can define a proactive care plan for each resident, areas of data collection, and team collaboration to keep the focus on improving outcomes, while decreasing resident and community costs.
The most valuable part of objective data and measures is that they are objective. Developing a strategic plan for data collection and analysis will support the proactive care plan by eliminating the subjective review of each resident.
Track Measures
It is always important to have resident and family feedback on how the PIP is improving the resident’s quality of life.
It is equally important to consistently track objective measures and quality indicators that are put in place, so there are triggers that warn the staff if a specific plan is not working for a resident. For example, Functional Outcome Measures (FOMs) for physical and occupational therapists are evidence-based tests that allow therapists to track the functional and cognitive status of a resident.
These tests are standardized, with clearly defined thresholds, allowing for easy access to baseline scoring and the ability to replicate, so each resident’s progress toward their goals can be closely monitored.
By effectively sharing resident outcome data with the team, an updated care plan can be created to avoid risk of decline or injury to the resident, while keeping their goals and dignity at the forefront of the conversation. Additionally, data collection from both internal and external team members will break down the barriers that may have limited communication in the past, allowing the focus to remain on the well-being of the resident, while lowering the overall cost of care.
The Next Step
Whether a facility is new to QAPI or looking for areas of improvement, the first area to examine is the PIP team. In order to be an effective team and achieve the culture shift of proactive care, members require the proper training, tools, and leadership.
With the support of the governing body, a clear direction can be defined that, in turn, makes everyone accountable for the dignity and well-being of all residents.
Bill Lampe, PT, DPT, MS, is clinical director, United States, Personal Care - North America, at SCA Americas. He can be reached at Bill.Lampe@sca.com or (215) 809-9672![Call: (215) 809-9672]() .
.