For coordinators at Professional Home Health Care (PHHC), a Boulder, Colo.-based home health agency serving more than 700 individuals across the state, tracking clients after they had been admitted into a hospital had become something of a game of hide and go seek.
Since PHHC staff didn’t always know where their clients had been admitted, they would first have to call around to as many as eight different hospitals. After tracking them down, they then would have to make another series of calls to learn who would be responsible for their discharge.
A Time-Intensive Process
Once staff secured the discharge planner’s contact information, they had to make regular calls to check on their clients’ status, ask what treatments or medications the hospital was administering to them, and find out when they were expected to go home.
“The entire process from start to finish took about 10 hours for every client,” says Alexis Bellinger, a care coordinator and registered nurse at PHHC.
Everything about that process changed after PHHC, by means of a health information technology (HIT) challenge grant, joined a long term care transitions program offered by one of Colorado’s state health information exchanges (HIEs). Through its access to a Web-based patient information data bank, PHHC is able to query each hospitalized client, find out where he or she is receiving care, review hospital charts, and get information on discharge status.
“Now we can actually log in and get that information in closer to 10 minutes,” Bellinger says.
Government Steps In
With the strong incentive of federal law, the health care industry began incorporating HIEs in 2002 upon release of final rules and regulations the Department of Health and Human Services (HHS) promulgated after passage of the Health Insurance Portability and Accountability Act (HIPAA) of 1996.
That law set up industrywide standards for coding medical procedures and gave patients a bill of rights over disclosure of their electronically maintained personal health data toward an effort to reduce the cost of health care, improve outcomes, and protect patient medical records from unauthorized use.
Regulations finalized in 2013 after passage of another HIT law offered additional guidance to providers on how to design interoperable data exchanges. Its rules also featured financial incentive programs to providers to help mitigate the cost of the massive industry shift from paper-based recording to electronic health records (EHRs).
But long term/
post-acute care (LT/PAC) centers, along with behavioral health and safety net providers, aren’t eligible for incentives. These groups were excluded in favor of those regulators felt had greater influence on health care delivery. For this and other reasons, they’ve lagged behind other health care sectors in setting up EHR systems.
Even as national statistics on EHR adoption rates across the LT/PAC community aren’t available, a March 2012 study reported in the journal Health Affairs found that only 6 percent of long term acute-care hospitals and 4 percent of rehabilitation hospitals had a basic EHR that would give providers access to patient demographics, problem lists, medication histories, clinical notes, electronic prescription orders, and laboratory and imaging results. Of the LT/PAC facilities that have a basic EHR, most aren’t equipped to trade data with the outside providers that are part of their residents’ extended care team.
Agency Brings LT/PAC Aboard
Realizing that LT/PAC facilities have been a missing link to HIT exchanges, especially when it comes to transitioning patients between nursing homes and hospitals, HHS’ Office of the National Coordinator for Health Information Technology (ONC), in collaboration with local HIE groups, has been researching EHR adoption and interoperability issues for LT/PAC providers in search of solutions to bringing them into the
fold.
Created in 2004 to coordinate electronic use and exchange of health information across the country, ONC in 2011 awarded $1.7 million in challenge grants to a state HIE covering parts of Colorado and similar groups in Oklahoma, Maryland, and Massachusetts for projects that would improve health data sharing between hospitals and LT/PAC providers during patient care transitions.
The Centers for Medicare & Medicaid Services (CMS) defines transition of care as the movement of a patient from one care setting, such as a hospital, ambulatory primary care practice, specialty care practice, home health, or LT/PAC facility, to another. LT/PAC residents might be admitted to a hospital for any number of reasons, including emergency treatment after an accident, routine treatment for individuals with chronic illnesses, or continuous care for patients with degenerative disorders.

“For us, the inclusion of the long term, post-acute care community with the health information exchange infrastructure stood out as one of the key challenges that the whole country was going to be looking at once the kind of basic infrastructure was laid,” says Kory Mertz, ONC challenge grant director.
Four States Make Plans
In Oklahoma, grantees worked with five nursing homes to develop an infrastructure to support electronic information exchange. In Maryland, grantees started out working with three long term care providers that were heavy adopters of HIT, then switched their focus to help smaller providers develop basic EHR systems.
The group in Massachusetts worked to identify the type of data LT/PAC providers needed in care transitions and moved toward developing standard procedures to capture this information. Colorado already had established two regional HIEs.
“Their goal out there was really to take long term and post-acute care providers in three different communities and have them connect up,” Mertz says. “They focused on communities where they had hospitals already participating in their health information exchange and worked to bring in various LT/PAC facilities.”
Colorado Accepts The Challenge
CORHIO, Colorado’s designated entity for an HIE for the eastern region, collaborates with physicians, hospitals, clinics, public health, LT/PAC, laboratories, health plans, and patients to improve care collaboration through secure systems and processes for sharing clinical information.
Toward that effort, it has established PatientCare 360, a health data portal accessible to subscribers through the Internet. It began inviting long term care facilities to apply to participate in its LT/PAC transitions program in April 2012.
For Pamela Russell, the long term care development outreach manager at CORHIO, the three-year project started out with surveys and PowerPoint presentations. CORHIO scoured the eastern part of the state and its rural areas, reaching out to skilled nursing facilities, assisted living, home health, hospice, and long term acute-care hospitals to study their current workflows for transitioning residents, learn how much time it took to gather the information, teach them about HIT, and invite them to participate.

Like PHHC, most facilities were exchanging information on transitioning patients through paper documents, faxes, and email. For LT/PAC providers, gathering all of the relevant data related to a resident’s care transition could take several hours.
“We wanted participating LT/PAC centers to have the information within two hours, and we wanted the facilities to be able to provide the required continuity-of-care document, which is a 90-day summary of treatment, to the individual or a family member upon request,” Russell says.
Grants Make Progress Possible
With the ONC challenge grant, CORHIO was able to waive the initial set-up and training fees, as well as monthly fees between $150 to $300 depending on facility size, for LT/PAC providers to exchange data, query patients, and review real-time updates of their residents’ health status. The data on PatientCare 360 ranges from hospital admission and discharge reports, lab reports, transcribed notes, to radiology reports.
“This tool allows them to access some of this clinical data without necessarily having a sophisticated electronic health records system in their office at their facility,” says Brian Braun, CORHIO chief financial and strategy officer.
 “That’s what we’ve found to be very useful for the long term care facilities, since many of them don’t have the types of systems that other providers have. It’s low-tech as far as access and getting information, but it has a high level of value as far as the information that’s in it,” he says.
“That’s what we’ve found to be very useful for the long term care facilities, since many of them don’t have the types of systems that other providers have. It’s low-tech as far as access and getting information, but it has a high level of value as far as the information that’s in it,” he says.
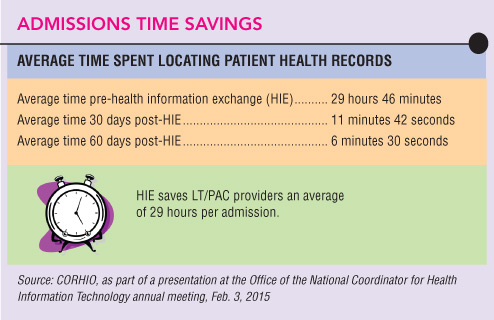
By January 2014, CORHIO had recruited a total of 119 long term care facilities, including 64 skilled nursing facilities; four assisted living facilities; 35 home health organizations, including PHHC; 14 hospice organizations; a long term acute-care hospital; and a long term care-specific lab. Overall, CORHIO found that the average time to collect relevant data on each patient dropped from 29 hours to six minutes.
“It makes an incredible difference in the accuracy and the timeliness [in which] we deliver information,” PHHC’s Bellinger says.
Information Flow Aids Care Planning
Three coordinators at PHHC are authorized to access PatientCare 360 to view updates on their clients and share care summaries with nurses in the field responsible for their clients’ care. The real-time information helps the six-location home health agency adjust care plans based on its clients’ conditions following their hospital stays.
“Let’s say there’s a change in the hospital where our diabetic client goes and then the next thing we know—worst case scenario—they have a leg amputation,” Bellinger says. “We can start prepping and say, ‘We are going to need physical therapy services. We are going to need occupational therapy.’ We can actually change our care plan while they are still in the hospital to accommodate the client better and also assist the hospital,” she says.
Even as grants covering subscription fees for CORHIO ended March 2014, PHHC will maintain its access to PatientCare 360, Bellinger says.
Interoperability Still An Issue
In addition to lower rates of HIT adoption among the LT/PAC community, other factors are holding up seamless patient health data exchanges between providers. One of the biggest is that the EHR systems the profession is using still don’t communicate.

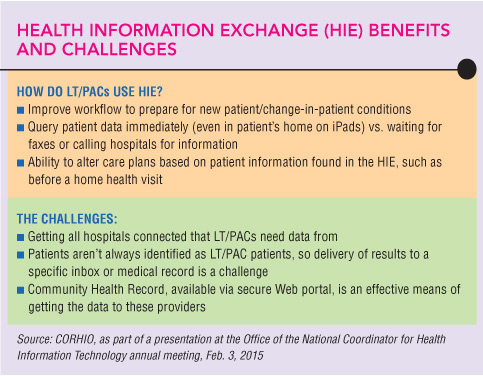
“I think one of the challenges that we’ve learned through our grantees, and also when talking with stakeholders generally, is that even when they do [want to] adopt an EHR, generally the EHR products that are available right now don’t necessarily include a functionality that supports interoperability,” says Liz Palena Hall, LT/PAC coordinator at ONC.
Vendor adoption of interoperable functionality for LT/PAC has been slow and uneven due, in part, to the fact that the LT/PAC community isn’t eligible for the Medicare and Medicaid EHR incentive programs, ONC said in a 2013 report on the status of health information in LT/PAC settings. “We are trying to educate both vendors and providers about what’s needed and also to think about who are their trading partners to understand the key pieces of information needed between the sender and receiver,” Hall says.
At the end of January, ONC released a draft interoperability road map to serve as an action plan for public and private stakeholders to move the profession toward greater sharing of HIT. The comment period on the plan extends through April 3.
Collaboration Needed
To support interoperability, Coral Lindahl, an EHR coordinator and PointClickCare liaison at a seniors housing community in Minnesota, says LT/PAC EHR software vendors need to come together to integrate patient record systems.
In January, Lindahl was in the final weeks of managing an 18-month special innovation project funded by Stratis Health, a Bloomington, Minn.-based nonprofit that works with CMS to foster collaboration and innovation in health care quality and safety.
The Health Information Technology for Post Acute Care (HITPAC) project connected hospitals with skilled nursing facilities and pharmacies in Minnesota. Prior to the project, some facilities were photocopying 30 to 40 pages of health care data and sending them with each resident who had to make a trip to the hospital.
“The hospital said, you know what? We don’t even look at that stuff. We don’t have time to look at it,” Lindahl says. As a result of HITPAC, facilities now transmit four or five pages of data about the patient, including a continuity-of-care document.
Some facilities plan to continue the live information exchange. Others are seeking funding to have their software vendors improve their continuity-of-care documents or produce the care summary. Still, Lindahl says, the long term care community in her region needs more support from hospitals to achieve success. “Even though [the hospitals] are saying, ‘We want to do this,’ we’re having trouble getting them to sit down at the table,” she says.
Transitions, Readmissions The Big Issues
There is a financial incentive for hospitals to meet long term care facilities halfway. Under a program to reduce the number of patients with certain illnesses returning to hospitals after treatment, HHS in October 2012 began penalizing hospitals for excessive readmission of long term care patients with heart disorders or pneumonia within 30 days of being discharged following a prior visit.
Under the Hospital Readmission Reduction Program, Medicare payments for acute-care hospital patients will be reduced 3 percent in fiscal year 2015 for excessive readmissions. HHS created the program to encourage hospitals to coordinate care with LT/PAC providers.
About 20 percent of Medicare patients discharged from a hospital are readmitted within a month, and 40 percent of these readmissions are from long term care facilities, according to HHS.
Reconciling Medications
Reducing avoidable readmissions also was one of the goals for the Minnesota special innovation project. HITPAC worked to reduce readmissions due to conflicts with medicine prescribed during a hospital stay and the resident’s ongoing prescriptions.
“What we found is that 65 percent of readmissions to the hospital in less than 30 days were related to medication issues,” Lindahl says. This is due in part to the differences between how hospitals and skilled nursing facilities record the reasons for prescribing a drug in the patient’s chart, she says.

Another problem prior to HITPAC was that when a resident returned home from the hospital, facility nurses were often left to determine whether the new prescription would interact with any other medicine the resident was taking. For some patients, the decision to administer or not administer a newly prescribed drug created another event where the patient had to be readmitted to the hospital.
“What we were trying to achieve was to get those drugs to a pharmacist first, have the pharmacist review them, tell us what was wrong with them, and then send them back to the hospital to get corrected [before sending the patient home] so that it would be a cleaner and safer hand-off of that resident to the next care transition team,” Lindahl says.
Despite the challenges for the long term care community, Lindahl, who has worked in health care for more than three decades, is hopeful about the future adoption of technology.
“When Alexander Graham Bell invented the telephone and he said, ‘Watson can you hear me?’ it’s the same thing,” Lindahl says, describing what it felt like when her team first transmitted live patient data to one of the hospitals in their community.
“But if you only have two people that have a telephone, there’s really no value. So we need for all these health care providers to start getting on their telephones so we can all start talking.” ■