When it comes to the mental health of individuals in long term/post-acute care (LT/PAC) settings, providers play a tremendous role. “All aspects of care and services in a LT/PAC center can contribute to overall well-being, including physical, mental, and social,” says Holly Harmon, senior director of clinical services at the American Health Care Association (AHCA). “Providers are expected to provide necessary care and services to attain or maintain a person’s highest practicable physical, mental, and psychosocial well-being, in accordance with the person’s comprehensive
assessment and plan of care.”
According to the U.S. Department of Health and Human
Services, mental health encompasses an individual’s emotional, psychological, and social well-being. The National Alliance on Mental Illness defines a mental health illness as a condition affecting a person’s thinking, mood, or feeling and may affect a person’s ability to function and relate to others. Research suggests multiple causes of mental health conditions, including genetics, environment, lifestyle, and even basic brain structure.
The elderly make up a significant share of the population with a mental health illness. According to the National Council on Aging, about one in four individuals aged 55 and over experiences a behavioral health disorder, with depression and anxiety disorders among the most common. Conditions like schizophrenia and bipolar disorder are also present, and while they are less common, they present significant functional impairments in the elderly population. LT/PAC experts say that incidents of post-traumatic stress disorder are increasing as it becomes more recognized.
Confronting a Stigma
“Mental health is still very stigmatized as a society, which makes it very hard,” says Lindsay Schwartz, PhD, senior director of workforce and quality improvement at the National Center for Assisted Living (NCAL).

“For diabetes, you can see that the blood sugar is high, or with congestive heart failure you can see that someone maybe is short of breath or retaining fluid. But, in things like depression, someone may exhibit symptoms like not talking, not wanting to eat, or feeling isolated,” she says.
Though the societal stigma is alive and well today, it was even stronger in the past. During her career as a case manager, Schwartz noticed an elderly patient’s records noted that she was taking an antidepressant. When Schwartz acknowledged her depression diagnosis, the patient strongly denied it. “We think of mental health as a stigmatized topic, but for the elderly it’s way more stigmatized,” Schwartz says. “It’s really impeding the care we give as health care providers. That is something as a society we need to think about and that needs to change.”
The Challenge for New Residents
Richard Juman, PsyD, national director of psychological services at TeamHealth, says the prevalence of depression in long term care is astronomical, and it is not difficult to understand why.
Newly admitted residents may struggle with myriad losses, such as health status, ambulation, home, community, activities—essentially most of the elements of the life they were leading. But it goes well beyond that, Juman says, because each resident is now challenged to create the most positive “final chapter” for themselves.
“So it’s really an existential process that involves each resident working on identity issues, like ‘Who am I now, and how can my life have meaning in my new situation?’ We want residents to become fully engaged in their new environment, to create meaningful connections with other residents, to actively engage in activities, and to get out of bed each morning with goals they would like to accomplish,” he says.

Unfortunately, many residents become too depressed to accomplish these goals, so the task at hand is to treat the depression and mobilize all of the residents’ psychological resources so they can rise to the challenge, Juman says. “Someone new going into assisted living or skilled nursing has had a major life change, and it could be just situational depression, but it still needs to be addressed,” says Schwartz. “Even more so in this case, because depression and other mental health conditions can really exhibit themselves in physical illness.”
While some residents may become depressed upon admission, says Juman, others exhibit challenging behaviors. Some centers may struggle to manage the anger, noncompliance, and other challenging behaviors that these individuals display. Consistent response from staff can be arduous, he says.
“Residents who manifest challenging behaviors may be angry, personality disordered, or chronically mentally ill, but there is another group in which these behaviors are common—residents who demonstrate the behavioral symptoms of dementia.”
Approaching Dementia Differently
The Diagnostic and Statistical Manual of Mental Disorders, a classification and diagnostic tool by the American Psychiatric Association, was released in May 2013. It classified dementia under a new category called neurocognitive disorder. This new classification differentiates dementia from other mental disorders, but for the LT/PAC profession, some linkages remain.
Historically, individuals with chronic mental health illnesses have been treated with psychotropics, and, in particular, antipsychotic medications. But with health care professionals’ current focus on reducing the off-label use of antipsychotics, LT/PAC centers are now finding that nonpharmacologic interventions are indispensable, says Juman. “In reality, nonpharmacologic approaches that involve direct clinical work with residents, in conjunction with psychologists working with facility staff to create behavior management plans, are much more effective, and less costly, in the long run.”
These efforts have also changed past paradigms about appropriate treatment and understanding of the behavioral expressions exhibited by individuals with dementia, says AHCA’s Harmon.
Studies have demonstrated that antipsychotic medications provide a small benefit for a limited set of individuals with dementia, but pose a large risk of adverse events. In 2012, the Centers for Medicare & Medicaid Services (CMS) launched the National Partnership to Improve Dementia Care in Nursing Homes.

AHCA supported that effort and set its own goal of a 15 percent reduction in the off-label use of antipsychotics for its members. That goal was achieved by the end of 2014, and in September of that year, CMS, AHCA, and others set new goals to continue reducing the use.
When staff in centers learned that the approach they were taught or had been practicing for some time in using antipsychotic medications for some individuals was unnecessary and potentially causing harm, there was an immediate response to change that practice, says Harmon.
“It makes me think of Maya Angelou’s quote, which goes something like: ‘We did the best with what we knew; when we knew better, we did better,’” she says. “This is exactly what happened with this effort. The dedication of centers across the country over the past several years has only strengthened to continue to change practice, improve quality of care, and quality-of-life outcomes.”
This campaign also brought focus to the necessity of practicing in a person-centered way, which is not only critical in caring for those with dementia, but critical to care and services for people with a mental illness. “It has shown us that rethinking what we do and how we do it is not only valuable as professionals, but can change the world for the people in our care,” Harmon says.
Caring for Residents with Schizophrenia
Dayspring Village, a licensed 96-bed limited mental health assisted living community located in Boulogne, Fla., has cared for a number of patients with both dementia and schizophrenia.
“One of the emerging things that we’ve seen is the co-occurrence of schizophrenia and early stage Alzheimer’s,” says Douglas Adkins, Dayspring’s executive director since 1989. “As people with schizophrenia get into their early 60s, there is a body of evidence that shows the early onset of dementia and schizophrenia arising at the same time. It’s a real conundrum for much of the long term care industry,” he says.
Caring for adults with schizophrenia and schizoaffective disorders, Dayspring offers custodial care, residential care, and support services.

The center has a cooperative agreement with a local community mental health agency, with six full-time mental health case managers assigned to the residents. Each resident works with their assigned case manager and facility staff to develop a community living support plan that details services to be provided, who will provide the services, and how frequently.
A typical resident at Dayspring is younger than a resident in a typical assisted living center, around 48 to 50 years old, and they have diminished insights due to the cognitive deficits presented by their schizophrenia or schizoaffective disorder.
“They get that one plus one is two, but they don’t get that one plus one plus one is three,” says Adkins. “They don’t get that integrated complexity, and it diminishes their capacity to acquire the insight that most people have. This results in poor decision making often and poor choices.”
Taking Control of Symptoms
Since 1989 to present day, Dayspring Village has cared for 3,800 residents. The key to their successes, says Adkins, is getting good control of the symptoms. “I don’t get too hung up on the diagnosis,” he says. “What I focus on is who you are as a person and what your symptoms are and what symptoms get in the way of you being successful.”
And success, he says, is often defined by the resident. For example, if a resident wants to go down to the local pond and catch a fish but his symptoms are in the way of his achieving that, Adkins and his staff focus on helping the resident get good control of those symptoms. “If we can reduce those symptoms and help you improve the quality of your life, then we can help you succeed,” he says. “And we want everyone to be successful.”
What Dayspring staff do not do, says Adkins, is treatment. That responsibility is reserved for the mental health professionals that partner with the facility, per the specialty license legislation created in 1996 that, among other things, separates responsibilities for housing and treatment.
Dayspring staff communicate and transfer knowledge about the residents to the targeted case managers and treatment professionals, so that they can update the plan of care and respond as needed. “This all improves the coordination of services, which lets us get better control of those symptoms and improve the capacity for these individuals to reside safely and appropriately in the community and achieve success,” says Adkins.
First and Foremost, Trust
But all of the staff’s efforts and treatments by mental health professionals would be futile without an essential element: trust. For residents with a mental health illness, reluctance to trust in staff members may stem from personal experiences in the mental health system that were not positive, and for many, it stems from the conditions presented by the disorder.
Stigma also plays a role, says Adkins. “Who wants to talk about how they feel from a mental health perspective?” he asks. “No one. So if you get an individual who’s had a bad experience, it can be very tough to make progress.”
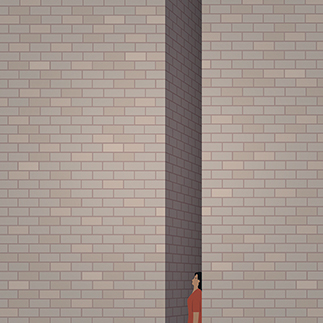
To gain trust, it’s essential that residents have individuals they can relate to. “There is a real wall there, especially with African American men and engagement,” he says. “Once you get them engaged and they know it’s OK, that no one is going to hurt them in any way, they can feel safe in sharing and no one is there is to lock them up. You will be surprised at how the process opens up. This takes face-to-face contact and time to build the relationship between the staff and resident. You must absolutely work at it.”
Adkins says that staff are focused on cultivating relationships with the residents, actively seeking them out. “Just as there are significant barriers to entry and participation, there are significant gains and significant recovery.”
Caring Holistically
Birmingham Green is a campus based in Northern Virginia that operates three different care centers. These include the Northern Virginia Health Care Center, a skilled nursing center that is licensed for 180 individuals, and two assisted living facilities: Willow Oaks, with 92 supportive housing units, and the District Home, which is licensed for 64 individuals. Residents range from 33 to 103 years of age. The campus has a strong history of caring for the neediest of the needy; that is, those with limited financial resources.

About 67 percent of the residents at Northern Virginia Health Care Center have a mental health diagnosis, and the number is 80 percent at Willow Oaks and 90 percent at the District Home. Some of the most common diagnoses are schizophrenia, bipolar disorder, anxiety disorder, and depression.
Joan Thomas is chief clinical officer for behavioral health, director of community relations, and administrator at the District Home. With a majority of residents in all three centers living with a mental health condition, she says, Birmingham Green approaches each and every one holistically.
“Caring for someone with a mental health challenge really is no different than any other type of challenge,” she says. “We want to do away with stigma. We really look at a person’s strengths. And our social workers and nursing staff are very attuned to individual needs.”
The main goal, she says, is to keep residents as independent as possible for as long as is possible.
One-Stop Shop for Care
If keeping individuals as independent as possible is the goal, offering multiple services under one roof is one way to go. The campus, which embraces the Eden philosophy, has a medical director of psychiatric service on staff and a psychologist who supports empowerment groups for skilled nursing residents, encouraging them to take control and run the group activities. Both professionals support residents’ case management.
The assisted living communities have social workers and support groups on site, which are designed to meet residents’ needs. The organization has also tapped into mental health interns, who do everything from designing a new yoga therapy program to carrying out music studies with the residents.
Staff Training a Key Ingredient
Thomas says that staff training has been a constant factor in helping residents maintain independence. The organization has adopted the HEAR model, designed by Andrew Heck, PsyD, cofounder, partner, and geropsychologist at GeroPartners. HEAR stands for health, environment, approach, and resident.
“We design a plan of care based on these components, and we look at the health of the person,” says Thomas. The staff ask various questions based on the four categories. Questions about the environment may include: Is it too cold? Too dark? What is happening in the environment that may impact the person?
For starters, staff assess how they are approaching the resident as a person and review their tone of voice, for example. Staff also seek to know the residents, their unique likes and dislikes, says Thomas.
“The HEAR model is a tool that offers our staff an opportunity to provide the very best service they can,” says Thomas. “It’s allowed us to look at residents in a cohesive manner. If someone is unhappy in the evenings, we ask, ‘What could be the trigger?’ Maybe it’s the radio or someone is talking too loud.”
Words of Wisdom
A top recommendation for providers wanting to focus more on mental health illnesses is to make sure there is a solid partnership in place with a mental health provider, Adkins says.
“Make sure you have partnerships built with the mental health partners that are motivated and interested in collaboration,” he says. “Don’t look for those who will just give you ancillary, casual support, but for those who will really get engaged as partners. When you have motivated partners, you get the needed energy for success.”
“It helps to work with geriatric psychiatrists if you can,” says Schwartz. “They are hard to find, because they are in a very specific field. If you can’t, try to find a psychiatrist and a geriatrician that are willing to work together.”
Harmon suggests that providers challenge themselves to be open-minded and to question their own biases. “It helps to challenge your own thinking and assumptions. Know each person’s strengths and abilities, and focus on those versus focusing on their deficits,” she says.
Thomas agrees. “There are ways to manage symptoms,” she says. “There’s a gentleman in our center who has chosen not to take medicine. He deals with his condition by painting. He’s painted murals, so if he wants to paint, we’re going to make sure he has a wall.”