Impact of the Pandemic on SNF Admissions for Low Income and Low English Literacy Beneficiaries
Daniel Ciolek
9/1/2022
This is the fifth of a series of articles related to the implementation of a Patient-Driven Payment Model (PDPM) supported by examples of data trends reported by the Centers for Medicare & Medicaid Services (CMS), academic researchers, as well as analyses conducted by AHCA/NCAL. In this series, we will contemplate questions related to patient care delivery, outcomes, and payment model implications informed by observed PDPM data trends. For previous articles, visit providermagazine.com.
In the fiscal year (FY) 2023 Skilled Nursing Facility Prospective Payment System (SNF PPS) Proposed Rule, CMS issued a Request for Information (RFI) on Overarching Principles for Measuring Equity and Healthcare Quality Disparities across CMS Quality Programs. The goal of the RFI was to discuss key principles and approaches that CMS could consider when advancing the use of quality measure development and stratification to address these concepts across various programs. In the FY 2023 SNF PPS Final Rule, CMS summarized stakeholder feedback and indicated the input would be used to inform future measure development efforts.
As AHCA analyzed various Medicare claims, assessment, and other administrative data related to the implementation of the PDPM, it became clear that the COVID-19 pandemic and related public health emergency (PHE) created shifts in the social determinants of health (SDOH) and social risk factors (SRFs) characteristics of SNF Medicare Part A patients, which were most apparent in the early months of the pandemic. In this article we present examples of these shifts and discuss the potential implications of including equity and disparity data in future quality measure development efforts.
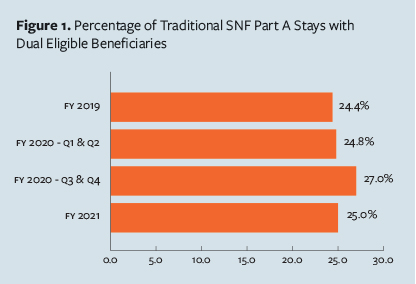 One indicator often used as a marker for income inequity is whether a Medicare beneficiary is also a recipient of Medicaid benefits (Dual Status). Figure 1 describes beneficiaries with traditional SNF Part A stays, and does not include admissions for patients with COVID-19 or patients admitted under the COVID-19 qualifying hospital stay waiver. As depicted in Figure 1, in FY 2019 and the first half of FY 2020 before the PHE (October 2018–March 2020), about 24.4– 24.8 percent of traditional SNF Medicare admissions were for dual eligible beneficiaries. During the first 6 months of the PHE from April through September 2020 (FY 2020 Q3 & Q4), the percentage of dual eligible beneficiaries increased to 27 percent, and then returned to near baseline in FY 2021 (October 2020–September 2021). We observed similar trends when looking at the percentage of zip codes below poverty level as well as zip codes with the lowest mean net worth.
One indicator often used as a marker for income inequity is whether a Medicare beneficiary is also a recipient of Medicaid benefits (Dual Status). Figure 1 describes beneficiaries with traditional SNF Part A stays, and does not include admissions for patients with COVID-19 or patients admitted under the COVID-19 qualifying hospital stay waiver. As depicted in Figure 1, in FY 2019 and the first half of FY 2020 before the PHE (October 2018–March 2020), about 24.4– 24.8 percent of traditional SNF Medicare admissions were for dual eligible beneficiaries. During the first 6 months of the PHE from April through September 2020 (FY 2020 Q3 & Q4), the percentage of dual eligible beneficiaries increased to 27 percent, and then returned to near baseline in FY 2021 (October 2020–September 2021). We observed similar trends when looking at the percentage of zip codes below poverty level as well as zip codes with the lowest mean net worth.
It is notable that during the first 6 months of the PHE, overall SNF admissions dropped precipitously; therefore, those admitted to a SNF during this period appear to have been those individuals less likely to have the financial resources or social supports necessary to permit a hospital discharge to home. When more was known about the COVID-19 virus and vaccinations were initiated, the relative percentage of dual eligible SNF admissions returned to near baseline.
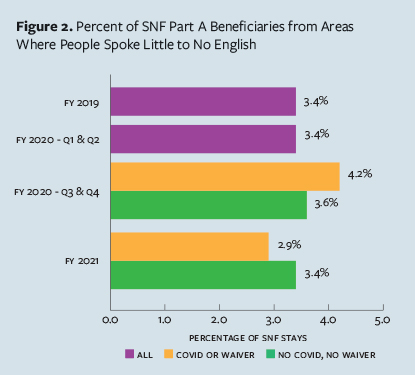 Another indicator often used as a marker for social inequity is preferred language or English proficiency. As depicted in Figure 2, In FY 2019 and the first half of FY 2020 before the PHE, about 3.4 percent of all SNF Medicare admissions (purple bars) were for beneficiaries from zip codes where residents speak little or no English. During the first 6 months of the PHE from April through September 2020, the percentage of beneficiaries from low English proficiency areas for traditional Part A admissions (green bars) increased slightly to 3.6 percent, and then returned to baseline in FY 2021. In contrast, during the first 6 months of the PHE, the percentage of beneficiaries from low English proficiency areas admitted with COVID-19 or under a PHE waiver (orange bars) increased to 4.2 percent, and then returned below baseline in FY 2021.
Another indicator often used as a marker for social inequity is preferred language or English proficiency. As depicted in Figure 2, In FY 2019 and the first half of FY 2020 before the PHE, about 3.4 percent of all SNF Medicare admissions (purple bars) were for beneficiaries from zip codes where residents speak little or no English. During the first 6 months of the PHE from April through September 2020, the percentage of beneficiaries from low English proficiency areas for traditional Part A admissions (green bars) increased slightly to 3.6 percent, and then returned to baseline in FY 2021. In contrast, during the first 6 months of the PHE, the percentage of beneficiaries from low English proficiency areas admitted with COVID-19 or under a PHE waiver (orange bars) increased to 4.2 percent, and then returned below baseline in FY 2021.
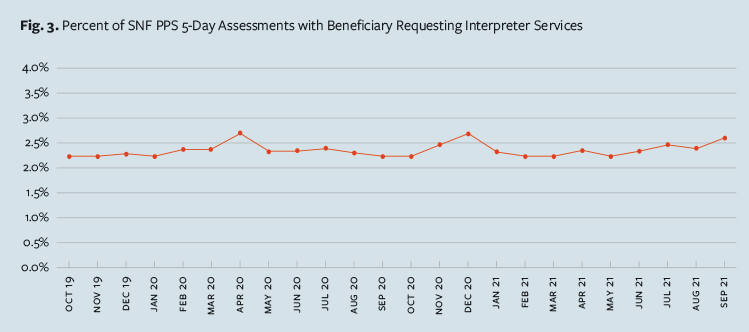
When considering all geographic locations, we observed a different pattern. As depicted in Figure 3, examining the month-to-month trends of SNF Minimum Data Set (MDS) patient SNF PPS 5-day assessment information of patients admitted without COVID in which the beneficiary requested interpreter services also revealed potential inequity impacts of the pandemic on people with low English proficiency. While the general trend for the need for interpreter services hovered around 2.2 percent, during the three significant COVID-19 surges beginning in March 2020, October 2020, and August 2021, the percentage of SNF Part A stays where the beneficiary requested interpreter services increased to around 2.7 percent.
While the absolute percentage changes in these examples appear to be small, when considered in a national perspective, the observed shifts can significantly impact the stability and accuracy of population-based SNF payment and quality measure models. Such impacts can be more apparent and can accelerate inequities in low-volume providers or in locations where these impacted populations are more densely concentrated if the models do not account for such shifts.
Indeed, from a payment policy perspective, CMS has considered the impact of the COVID-19 PHE-related shifting SNF admission demographics and took steps to minimize the impacts in its methodology to establish the PDPM parity adjustment adopted in the FY 2023 SNF PPS Final Rule. Similarly, CMS has revised the SNF Quality Reporting Program by modifying performance periods and adding COVID-19 risk adjustors and adopted temporary policies in the SNF Value-Based Purchasing Program to suppress unstable facility-specific performance scores due to the impact of the PHE.
As policymakers and the health care community explore the impact that SDOH and SRFs have on patient health and health outcomes, it will be necessary to identify those factors that can best address inequities and be responsive to sudden shifts in SNF patient care needs.
However, as AHCA stated in our FY 2023 SNF PPS Proposed Rule comments related to the CMS Measuring Equity and Healthcare Quality Disparities RFI, while we support the continued development efforts of measure concepts to address health equity and disparities across CMS quality programs, “we caution against advancing numerous and time-consuming structural and process measures that demonstrate an organization is good at ‘checking the box’ that they did what was asked on a quality measure checklist. We would prefer efforts be directed at exploring the thoughtful development of meaningful and risk-adjusted outcomes measures that demonstrate that the facility is showing progress at overcoming such historical barriers to quality care.”
Daniel Ciolek is associate vice president, therapy advocacy, for the American Health Care Association.