Changes in the Acuity of Patients Admitted to SNF After 3-Day Hospital Stay During Pandemic
Has there been a permanent change in the acuity of Medicare beneficiaries admitted to a SNF following a traditional 3-day inpatient qualifying hospital stay?
Daniel Ciolek
8/28/2023
In October 2019, the Medicare Part A Skilled Nursing Facility (SNF) payment model transitioned from the Resource Utilization Groups, Version 4 (RUG-IV) case-mix payment model, which focused on resource use, to the Patient-Driven Payment Model (PDPM), which focuses on patient characteristics. In the Fiscal Year (FY) 2023 SNF prospective payment system (PPS) Final Rule,1 the Centers for Medicare & Medicaid Services (CMS) implemented a 4.6 percent parity adjustment (phased in over 2 years) as the agency concluded the PDPM was not implemented in a budget-neutral manner.
Before finalizing the parity adjustment, CMS modified the approach based in part upon American Health Care Association (AHCA) analysis and comments on the impacts of the COVID-19 pandemic, which we referred to as COVID spillover. However, AHCA remains concerned that there has been a permanent change in the acuity of Medicare beneficiaries admitted to a SNF following a traditional 3-day inpatient qualifying hospital stay (QHS) that CMS must consider as the agency contemplates adjustments to the PDPM.
The below figures and discussion highlight some of the comments2 AHCA submitted to CMS in response to the CMS FY 2024 SNF PPS Proposed Rule3 based upon an analysis conducted by Avalere Health on behalf of AHCA. Specifically, Avalere identified SNF stays using 100 percent Medicare standard analytic files (SAFs) from October 1, 2019 to June 30, 2022. SNF stays with a diagnosis code or with a condition code signifying the stay utilized a 3-day acute stay waiver were not included in the analyses. Hospital claims were then identified to generate the trend charts reflected in Figures 1-3 for inpatient hospital Medicare Severity Diagnosis Related Group (MS-DRG) weight, QHS length of stay, and the percentage hospital discharges to SNF with inpatient complications and comorbidities codes.
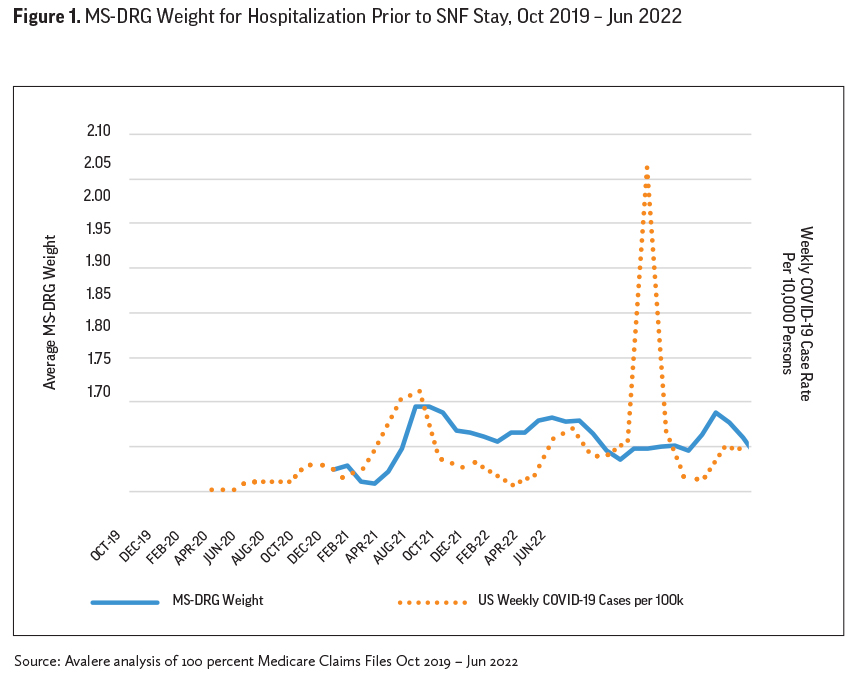
A strong indicator suggesting that the traditional SNF Part A population admitted following a 3-day QHS is different since the onset of the COVID-19 pandemic is the significant increase in the average MS-DRG weight derived from hospital discharge claims depicted in Figure 1. The MS-DRG weight increased significantly with the onset of the pandemic, and during the major subsequent case rate surge periods, and remains significantly elevated above pre-pandemic levels. Other Avalere MDS primary medical condition category findings discussed in the AHCA FY 2024 SNF PPS Proposed Rule comments2 provide supporting evidence of the notable and persistent shift upwards for higher acuity clinically complex conditions being admitted to SNF since the onset of the pandemic.
Figure 2 shows that with the onset of the COVID-19 pandemic, those beneficiaries that were admitted to a SNF following a 3-day or longer inpatient hospital stay had significantly longer inpatient stays than prior to the pandemic. The hospital length of stay increases spiked during COVID-19 case rate surges and remained elevated following the surges.
The increased duration of the hospital stay prior to SNF Part A admission could be the result of some combination of higher acuity patients and/or lack of availability of SNF beds. Regardless of the source of the increased inpatient length of stay prior to the SNF admission, it is well known that long hospital stays prior to a SNF admission are associated with additional clinical complexities or conditions acquired during the hospital stay. For example, incontinence and pressure ulcers can be the result of a long hospital stay, and the trends discussed in the AHCA FY 2024 SNF PPS Proposed Rule comments2 provide supporting evidence that the ongoing increased patient acuity for SNF Part A admissions than was observed prior to the pandemic might be related to the longer hospital stays prior to SNF admission.
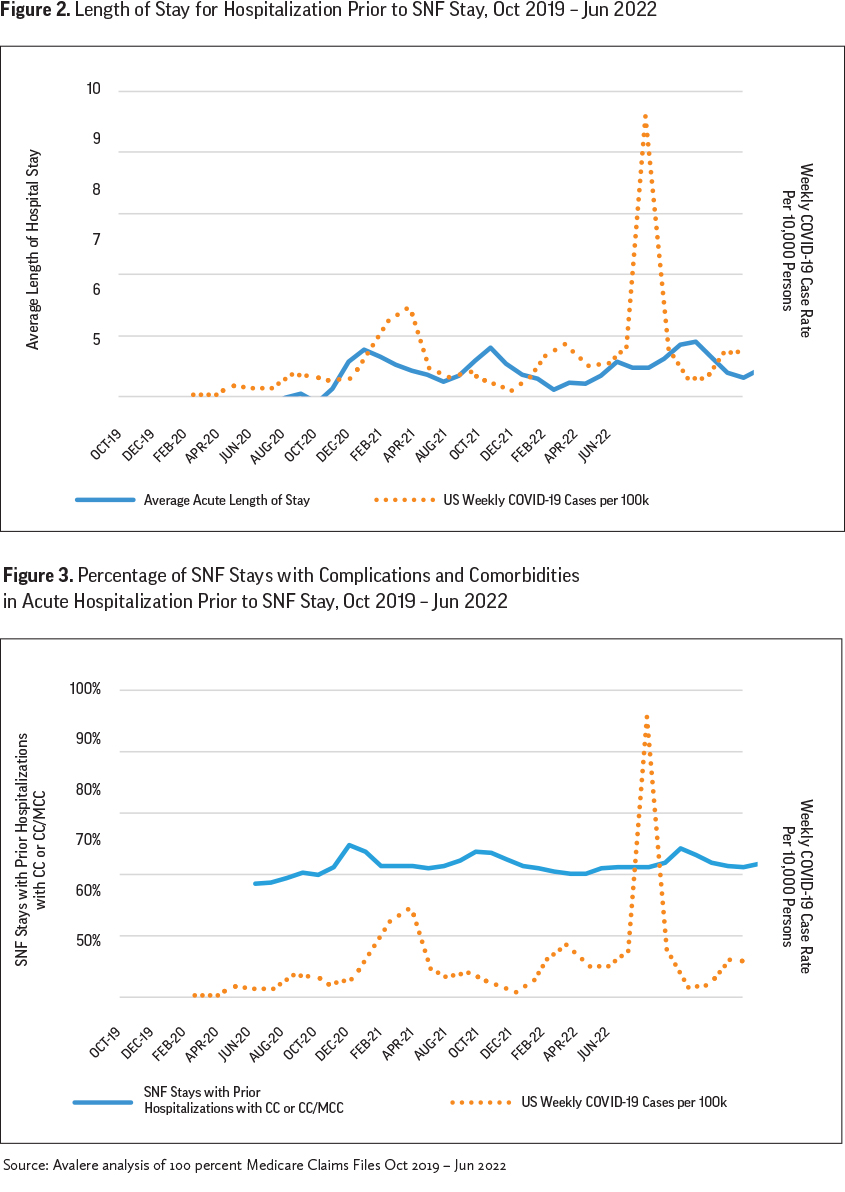
We anticipate that if the duration of inpatient hospital stays starts trending towards pre-pandemic levels, then the reported rates of incontinence, pressure ulcers, and other hospital-acquired conditions noted on the 5-day SNF assessment that elevate PDPM case-mix indexes (CMIs) will also show reductions.
A key driver of the MD-DRG weights for SNF admissions following a 3-day inpatient stay reflected in the Avalere Figure 1 trendline is reflected in the Avalere Figure 3 trend of percentage of SNF stays with complications and comorbidities (CC or MCC) in the acute hospitalization prior to the SNF stay. We note a strong parallel between the trendlines, suggesting that much of the increases in the MD-DRG weights are due to the increased presence of chronic condition comorbidities for SNF admissions since the onset of the COVID-19 pandemic, and that the acuity of patients being admitted to SNF following a 3-day inpatient stay remains higher than pre-pandemic levels. Such increased complexity has increased SNF PDPM CMIs since the onset of the pandemic, and they will unlikely return to pre-pandemic levels unless the trends of the hospital CC/MCC profile of SNF admissions return to pre-pandemic levels.
Conclusion
Prior to the COVID-19 pandemic, approximately two-thirds of Medicare beneficiaries that were able to be admitted to a SNF without a 3-day QHS were those in Medicare Advantage (MA) plans or those in accountable care organizations (ACOs). A recent CMS analysis4 demonstrated that the 3-day waiver use by ACOs reduced costs while maintaining outcomes. Another recent study5 under a CMS initiative demonstrated the potential of SNF skill-in-place waivers to reduce hospitalizations and improve outcomes for long-stay nursing facility residents.
With the expiration of the COVID-19 public health emergency (PHE) on May 11, 2023, beneficiaries not in a MA plan or an ACO are no longer eligible for the benefits of the 3-day QHS waiver and may instead require hospitalization, increasing out-of-pocket costs and increasing risk of hospital-acquired conditions. AHCA intends to conduct and share with CMS an ongoing analysis of trends discussed in this article related to the impacts on the clinical characteristics of traditional Medicare Part A SNF 3-day QHS admissions during the post-pandemic era.
References
1. https://www.govinfo.gov/content/pkg/FR-2022-08-03/pdf/2022-16457.pdf
2. https://www.regulations.gov/comment/CMS-2023-0048-0031
3. https://www.govinfo.gov/content/pkg/FR-2023-04-10/pdf/2023-07137.pdf
4. https://innovation.cms.gov/data-and-reports/2023/snf-waiver-summary
5. https://www.jamda.com/article/S1525-8610(23)00464-4/fulltext
Daniel Ciolek is associate vice president, therapy advocacy, for the American Health Care Association.