Nursing Homes, Person-Centered Care, and the 5Ms of Geriatrics
The 5Ms are giving care teams a clear, person-centered framework to improve life for residents.
Cathy Ciolek
9/9/2025
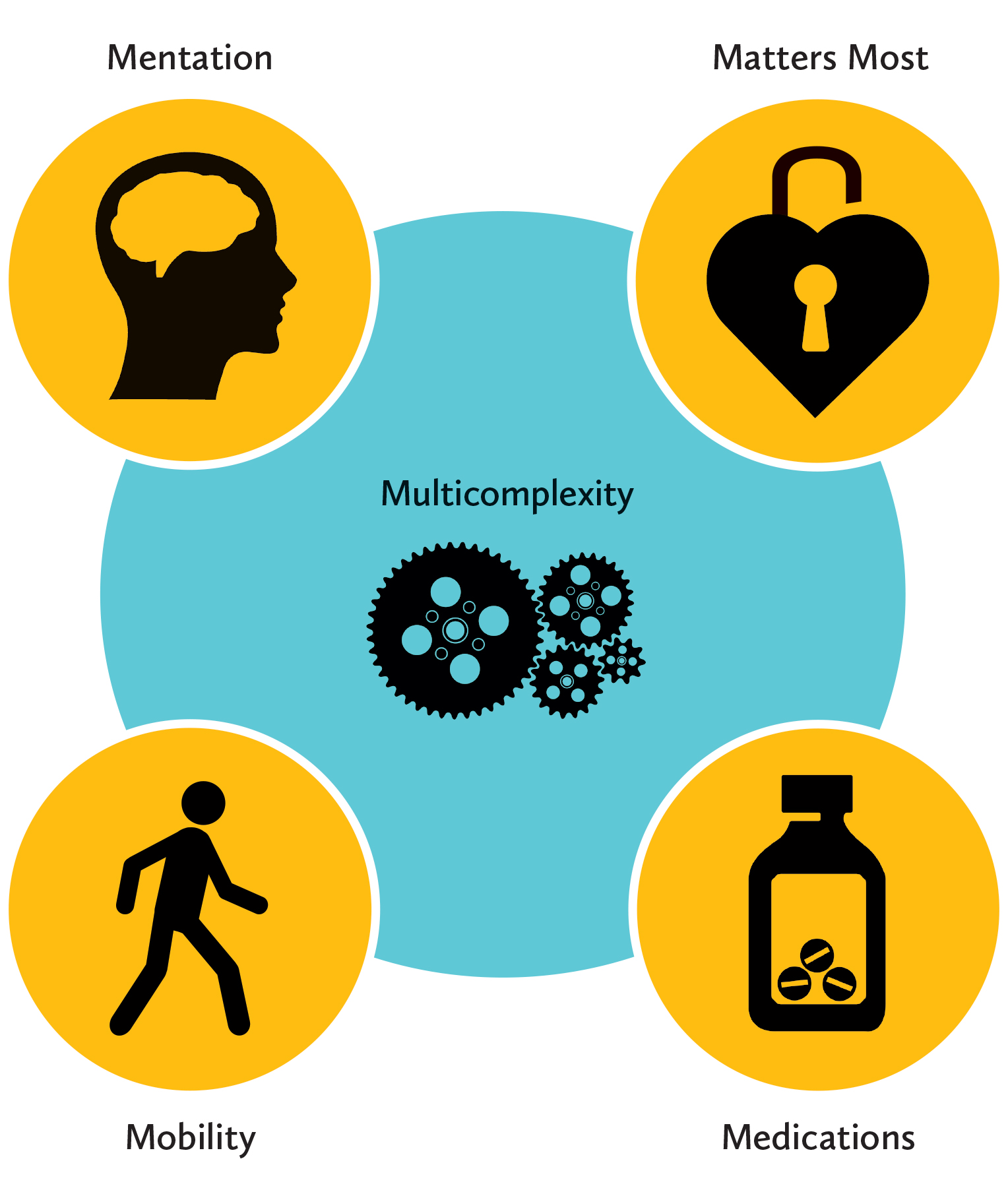
Person-centered care is at the heart of post-acute care. The Age-Friendly Health Systems initiative was established by The John A. Hartford Foundation and the Institute for Healthcare Improvement to transform health care to better serve older adults by focusing on a framework known as the 4Ms: what matters most to them, medications, mentation, and mobility. Many organizations, such as the American Geriatrics Society, American College of Physicians, and Academy of Geriatric Physical Therapy, recognize a fifth M: multicomplexity.
While there are several effective approaches to implementing person-centered care, the 5Ms framework is growing as a common communication structure across health care providers. Many of the professionals and health systems you work with may be adopting the 5Ms, and this can be a great way to connect care before and after a resident’s nursing home stay.
A recent study published in the Journal of the American Geriatrics Society of a Veterans Health Administration skilled nursing facility found that clinical outcome improvements were noted in documentation of life-sustaining treatment choices (what matters most), reduction in fall rates (mobility), decrease in “disruptive behaviors” (mentation), and deprescribing of medications. Additionally, the facility saw decreased rehospitalization rates and improved patient satisfaction scores.
 The good news is much of the care provided for older adults uses these principles, and building on them across disciplines is one way of advancing person-centered care.
The good news is much of the care provided for older adults uses these principles, and building on them across disciplines is one way of advancing person-centered care.
What Matters Most
This is the core of geriatrics care. Understanding what matters to residents in long term care or short-stay rehab is reflected in the care plans and health care decisions made every day. In rehabilitation, goal concordant care means the interventions must be related to functional goals, and these must be developed via shared decision-making with the resident. As a physical therapist, I can’t set a goal and expect the resident to participate in therapy if the task is not important to them.
For longer-term residents, the interdisciplinary care plan includes health goals, end-of-life care planning, and identification of health care proxies. These are not static and should be revisited as a routine part of care and when significant changes have occurred.
Medications
A medication review is part of every admission and conducted quarterly as part of the facility interdisciplinary drug-regimen review. Beyond reviewing what medications are administered and at what doses, the evaluation should entail an examination of all medications using standard evidence-based guidelines or protocols, including identifying potentially inappropriate medications specific to older adults.
In rehabilitation, the medication review can focus on what may be influencing mobility and mentation. Could the new medication be impacting the resident’s ability to participate in therapy? Is it impacting appetite and willingness to eat? Working with the pharmacy supplier and pharmacists who conduct a monthly review is a start, but nursing home staff and family know the resident best, and they should be able to identify how any new medication or change in dose impacts the resident’s day-to-day life and goals.
Mentation
Screening for cognitive or mental health issues is a routine part of admission and quarterly assessments. If there is a change in mental status, is it slow to progress, which may be a form of dementia, or quick, which may indicate delirium or a side effect of a medication or infection? Site transitions, moving rooms in the home, or transferring to a hospital are high-risk times for residents with delirium or dementia. Nursing assistants and environmental service staff who frequently interact with the residents may be the first to identify a quick change in mental status, so working with the entire care and support team for training and awareness is key.
Mobility
For many, mobility is a key feature of well-being. For nursing homes, finding the balance between supporting mobility and minimizing falls is the never-ending task. What level of risk is the resident (and family or legal representative) willing to take, and does the facility understand how that integrates with what matters most to the resident? Does the level of risk the resident is willing to assume match what the facility is willing to assume? Does it impact other residents’ safety and well-being? When caring for a frail population, it’s key to have these discussions early and often and be sure the care and support teams are aware. Documenting the discussion and care-planning the negotiated level of mobility should follow.
Also consider training the care team members to provide the right amount of needed assistance. This takes time knowing the residents, watching for fluctuations, and communicating any changing mobility issues.
Multicomplexity
The typical nursing home resident is considerably more complex than residents of twenty years ago. This makes providing evidence-based care difficult, as many of the clinical guidelines are single-disease or single-issue focused. It also means that treatment for one issue can have a large impact on another medical issue or life preference. Knowing what matters most to residents can help with managing mobility, medication, and mentation as people experience new problems or the need for palliative care.
 The 5Ms are significantly interrelated and require teamwork to monitor, update, and implement. They can help to break down the silos of professional expectations and be used to improve communication across care and service departments. Mobility is not just a rehab issue, and medications are not just for the referring practitioner and pharmacist. The exciting aspect of the move toward adopting the 5Ms is creating a consistent language on the key practices of care for older people. Having various discipline and health care systems speaking the same language will only improve care delivery, outcomes, and care transitions across services.
The 5Ms are significantly interrelated and require teamwork to monitor, update, and implement. They can help to break down the silos of professional expectations and be used to improve communication across care and service departments. Mobility is not just a rehab issue, and medications are not just for the referring practitioner and pharmacist. The exciting aspect of the move toward adopting the 5Ms is creating a consistent language on the key practices of care for older people. Having various discipline and health care systems speaking the same language will only improve care delivery, outcomes, and care transitions across services.
Cathy Ciolek is president of Living Well With Dementia, LLC, providing education and consultation to promote well-being and positive expectations for aging adults. She currently serves as president of the Academy of Geriatric Physical Therapy, which adopted the 5Ms as core principles for education and knowledge translation for its members.