
Long term and post-acute care (LT/PAC) has been behind the curve when it comes to employing metrics. But with the skilled nursing profession becoming more competitive, and with reimbursement rates being squeezed by new regulations and value-based care initiatives, making important decisions without analyzing relevant data is no longer a sustainable strategy.
A Powerful Platform
CarDon & Associates, a family-owned and -operated LT/PAC company with more than 2,000 patients cared for on a daily basis across Indiana, embarked on a culture shift to infuse data analytics into day-to-day decision making.
CarDon provides rehabilitation, memory support, long term care, assisted living, and independent living in 21 communities. The goals for the initiative were three-fold: improve the patient care experience, improve the overall health of patients, and reduce the per capita cost of care.
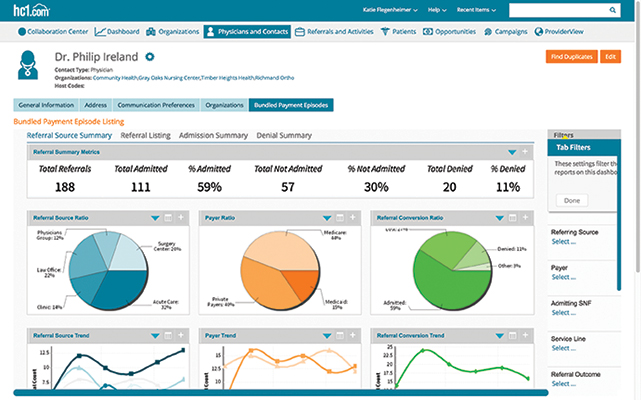
In 2017, CarDon activated an analytics platform that imports data from various sources, including electronic medical records, admissions/discharge, and staffing and supplies. The platform allows the provider to easily analyze the data for trends in near real time, while built-in alerts prompt staff to take action.
Use of the platform has grown. Today, it is widely used by the chief operating officer, regional directors, clinical officers, and marketing executives to make informed decisions to improve service and drive efficiencies in a number of areas.
Smoother Admissions and Discharges
Admission and discharge managers at CarDon’s various facilities thought they had a good idea about the timing of admission and discharge spikes, but without data, they were working with hunches.
The prevailing thought was that admissions where highest on Fridays from 4 to 7 p.m. After activating the analytics platform, managers found a similar spike on Wednesdays from 3 to 6 p.m. The data showed that these patients most likely were orthopedic patients who had surgery on Monday and were ready for rehab on Wednesday.
CarDon also now knows that the bulk of discharges happen from noon to 3 p.m., so discharges and admissions sometimes overlapped, creating unnecessary stress on nurses. To reduce this overlap, clinical personnel are able to use the analytics platform to work with specific doctors and hospitals to admit patients to CarDon facilities earlier so new patients can get the full attention they need before evening.
In addition, nurses can work with families to get current patients discharged earlier in the day, creating a better flow of admissions and discharges.
Finally, using the analytics platform, CarDon is able to view the average length of stay for specific admissions, which enables discharge nurses to begin having conversations with families at an appropriate time to ensure they are prepared for the patient to come home.
Improved Staffing
With a full understanding of admission and discharge trends, facility managers are able to staff more appropriately. For example, a review of staffing on Wednesdays showed that nurses and housekeeping staff were scheduled for 7 a.m. to 3 p.m. shifts. This meant that nursing shifts were switching just as orthopedic patients were arriving, which did not set the stage for a welcoming environment for new patients.
Likewise, with the bulk of discharges happening from noon to 3 p.m., housekeepers are busiest from noon to 5 p.m. cleaning rooms to prepare for new patients.
Managers agreed there was no reason to be fully staffed with housekeepers beginning at 7 a.m. since the bulk of their work takes place later in the day. CarDon managers were able to change the shifts of registered nurses, licensed practical nurses, and housekeepers to ensure a smooth transition for patients and a better working environment for staff.
Enhanced Patient Care
One of CarDon’s goals is to constantly become a better partner for referring facilities and doctors. With the help of the analytics platform, CarDon is now able to identify trends based on evidence that can be communicated to hospitals and physicians to provide value to the relationship and to drive better patient care.
For example, CarDon will be using this analytics platform to look at ways to reduce falls in the facility. If clinicians feel that patients are at risk of falling, it is easy to generate a report on patients who have fallen and look for common threads, such as medications. Trends can be presented to doctors, who are more likely to make changes to prescribing behavior with evidence-based research.
Key metrics from CarDon also can be used to pinpoint emerging health scenarios and to create workflows to act on before reaching an emergency. For example, if a patient’s blood pressure has gone down during four consecutive readings, CarDon can alert nurses to proactively take appropriate clinical steps to address the issue before it turns into a transfer to the emergency room.
Enabling faster decision making via alerts allows the clinical staff to focus on providing better care for the patient.
Reduced Readmissions
Readmission rates are a focus for all skilled nursing facilities (SNFs), so better understanding the data around readmissions is crucial to reducing their frequency. CarDon tracks exactly how many patients are readmitted to specific facilities, why these readmissions are occurring, and when readmissions are happening. By reviewing the information and highlighting trends and issues, CarDon can better understand the root cause of readmissions and serve patients better to prevent more readmissions from happening.
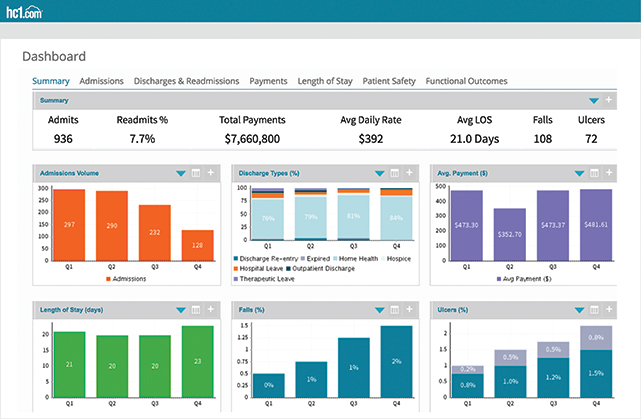
An example of how this works: A SNF found that 60 percent of patients with chronic obstructive pulmonary disease and heart failure with diabetes were readmitted to the hospital after the first week at the facility, and that readmissions happened between 10 a.m. and 3 p.m. Medical staff can now study this information to find out the underlying cause, asking questions such as what is happening during these dates and times, which hospitals are referring these patients, and what medications are these patients taking? By having access to this information, medical staff can make evidence-based decisions to reduce or eliminate these readmissions.
Changing a Mindset
The switch to a data-first culture takes time and a lot of communication. As with any LT/PAC organization, CarDon has experienced some pushback from management staff who felt their experience provided the evidence they needed to provide the best care.
However, as management staff have become exposed to the kind of detailed data available through the analytics platform, and how these data can be used to deliver even better care, they are embracing the change. CarDon is also considering using metrics for supply management and food waste reduction.
Brian Peters is chief information officer at CarDon & Associates. He can be reached at bpeters@cardon.us.