No reasonable person could have anticipated the stunning $677 million jury award levied against Skilled Healthcare Group last July for a case in which the plaintiffs did not allege any harm had occurred to any patient, says Mark Reagan, managing partner of Hooper, Lundy, and Bookman out of their San Francisco office. Reagan and partner Scott Kiepen were regulatory counsels for the Skilled Healthcare case.
Rather, the plaintiffs’ charge was that Skilled Healthcare’s 22 California facilities had failed to meet a purported regulatory requirement to provide an average of 3.2 hours of nursing care per patient per day, a charge the company still maintains is false.
Unexpected Results
In fact, attorneys involved in the case fully expected it would be dismissed. In 2007, the California Supreme Court in Alvarado vs. Selma Convalescent Hospital upheld a superior court’s dismissal of a similar class action case, holding that “calculating staffing pursuant to 1276.5 [a California Health and Safety Code that was also used in the Skilled Healthcare case] was better left to the administrative agency charged with regulatory oversight rather than trial courts,” says Kippy Wroten, lead trial counsel for the Skilled Healthcare case.
“For that reason it was felt that this judge would follow the wisdom of the Alvarado court, but obviously he did not.” Instead, not only did Judge Bruce Watson of Superior Court in Humboldt County, Calif., take the case, he exhibited behavior and made numerous rulings that caused defense attorneys to seriously question his impartiality.
Patient Harm Not The Issue
The case is disturbing on many levels, observers note, but perhaps the most disturbing aspect is that a case with no allegation of patient harm led to such a massive award. The plaintiffs’ primary allegation—that the company had violated a vague staffing statute—had no regulations as required by the statute, nor any legal precedents to back it up and help a court determine whether and in what way the purported staffing requirement should be enforced, defense attorneys say.
“Without legislative and regulatory change, you can expect to see more of the same type of
lawsuit in the future against other health care providers,” says Wroten.
“It’s a strange, sordid tale,” says Reagan. “I don’t think anyone, whether it was us or anybody else involved in this case, could have reasonably expected any outcome that was so aberrant and so outrageous given the facts here, by virtue of … the combination of a judge misunderstanding and misinterpreting the law and a jury taking [his] instructions and applying the maximum amount of damages,” he says. “It really turned existing law on its head.”
Long term care defense attorneys report that staffing regulations used as a foot in the door to sue providers is occurring with greater frequency, and it’s a trend that alarms them.
Attorneys See Disturbing Trends
Both in California and across the nation, Reagan says he has seen “an increased collapsing of the regulatory system in the civil liability system.”
This happened several years ago in Florida, he says, when an increase in
patients’ rights litigation resulted in so many lawsuits that insurers were forced to raise their liability rates to unprecedentedly high levels. The state saw an exodus of multifacility operators because they simply could not afford the dramatically increased liability insurance costs.
Although Reagan and Kiepen are hopeful that cases in other parts of the country will receive a more rigorous review of the law and face a more impartial judge than Skilled Healthcare confronted, Darren McKinney of the American Tort Reform Association expresses alarm. “It is and ought to be seen as a big warning horn. The storm is rising, it’s over the horizon, and if you don’t batten down the hatches” you might just get swept overboard, he says. The Skilled Healthcare case’s outcome “speaks volumes about where long term care litigation could go if policy makers don’t soon get a handle on it.”
“Very generally speaking, the plaintiffs’ bar has increasingly, for the last several years, begun to target long term care companies,” says McKinney. Personal injury lawyers are working at both the state and federal level, with legislators who are “bought and paid for,” says McKinney, to have legislation passed that would make it easier to bring lawsuits and to increase providers’ liability, “and so you’ve got not only legislative efforts under way, but the frequency of actual lawsuits against long term care providers has been steadily increasing.”
And staffing levels are increasingly being used to show that a long term care company was willfully negligent in its care for patients.
Staffing Levels Under Fire
Priscilla Shoemaker, legal counsel for the American Health Care Association (AHCA), is concerned that the litigation situation is returning to something like what it was in the late 1990s, when cases went all the way through litigation rather than being settled early on. The result was high jury verdicts with additional punitive damage awards that, in turn, drove liability costs so high in some states, such as Florida, Arkansas, and Texas, that some providers were forced to close their doors or divest themselves of facilities in those states.
“We’re seeing a new explosion of tort litigation resulting in jury verdicts for excessiveley high amounts,” Shoemaker says. And a key complaint being used to attack long term care companies in these cases, she says, is inadequate staffing levels.
The Skilled Healthcare decision is different from many recent cases in that there was no claim of any patient harm. But the focus on staffing is the same. In the more typical case today, harm is alleged and then blamed on understaffing, says Shoemaker. “There always seems to be this inference that staffing is not up to par,” she says.
The other trend that Shoemaker is seeing is that parent companies are being held liable along with their targeted facilities.
In July 2010, a Sacramento, Calif., court ruled there was “…overwhelming evidence of the corporate defendants [Horizon West] running their business based, time and again, predominantly on a concern for the bottom line on the financial reports instead of any focus on compassionate patient care.” No surprise, understaffing was alleged in this case, too, and the plaintiffs’ award was approximately $29 million, with $28 million of it in punitive damages.
Going After The Corporation
Perhaps the focus on staffing is precisely to take the case to the parent corporation, whose pockets are deeper, observers note. “Staffing is being argued as a fundamental corporate responsibility,” says Shoemaker. The corporation is supposed to know whether staffing is adequate. If it’s not, “that may be willful and intentional disregard for patient safety, which under some states’ statutes and regulations triggers the additional assessment of punitive damages,” she says.
In Pennsylvania, “we’re seeing staffing levels as a predominant theme” in lawsuits being brought against long term care facilities or companies, says Stuart O’Neal, a member of the Pennsylvania Health Care Association’s Tort Liability Committee and a private attorney defending medical malpractice and long term care cases throughout the state.
Pennsylvania is an attractive venue for some personal injury lawyers because it hasn’t had tort reform and has no caps on awards, says O’Neal.
“The baseline allegation,” he says, is that long term care organizations are putting profits over people—that “a facility will understaff intentionally, knowing that the quality of care will suffer,” he says. Regardless of the kind of case it is—be it wound care, failure to thrive, or slips and falls—“it’s the same kind of complaint over and over again where they focus on staffing levels,” he says.
Steps To Take
Long term care providers can protect themselves from these major jury awards in four main ways: providing quality care and meeting regulatory requirements, creating a system that ensures thorough and accurate documentation of every aspect of care and staffing, being prepared for possible testimony by ex-employees, and providing new residents the opportunity to sign carefully crafted alternative dispute resolution agreements, experts say.
1. First, do no harm.
It’s self-evident that the most important thing providers can do to keep from losing a lawsuit alleging negligence or abuse is to make sure that they are providing quality care and complying with all regulations. Because staffing levels are receiving so much attention, it’s important to make sure a facility is staffed appropriately for the facility’s acuity level, say attorneys, and that it always at the very least meets the state’s minimum requirements.
“Every provider needs to incorporate staffing requirements as part of its compliance program,” says Kiepen.
“One thing providers need to know is that any cracks in your regulatory compliance are potentially exploitable by trial lawyers; that is, trial lawyers are going to be looking for regulatory noncompliance just as regulators are,” says Reagan.
And to prove that compliance, accurate and thorough documentation is essential.
2. Documentation can win a lawsuit.
A good defense in the event of a lawsuit will require supporting documentation to prove that the facility did, in fact, comply with regulations, says Reagan. “There is a very high premium placed on maintaining accurate and supportable documentation.”
Providers would also be wise to evaluate the documentation systems they maintain and consider eliminating or augmenting certain documents to be sure plaintiffs’ lawyers cannot later misconstrue their purpose and use the documents against them.
For example, take a company that has internal documents, some of which are designed to provide operators with a general snapshot of a facility’s daily compliance and others of which are prepared later and take into account various operational issues so providers can track trends and confirm actual compliance. If they’re sued, the documents designed to merely provide a general snapshot of compliance can actually work against them.
Plaintiffs’ lawyers argue to jurors, who are unfamiliar with the intricacies of systems for tracking employee hours and patient census, for example, that the snapshot documentation is inaccurate—and providers find themselves arguing against their own documentation to defend themselves, trying to explain that the documentation was not designed to be used in the manner plaintiffs allege.
Teach Documentation Skills
Providers need to conduct frequent in-services on documentation, says O’Neal, so that details about things like when a resident received a bath, or when the resident left the facility to go to a hospital, for example, are written down and kept in such a way to make them easily accessible, even four or six years later.
If the documentation is “not filled out properly—doesn’t have the date or the time, or consists of very short and abbreviated entries, or doesn’t track pain appropriately, those are all easy targets for plaintiffs to latch onto and show injury,” O’Neal says.
If a resident has a fall, is transferred to a hospital, has a severe change in condition, or the family or physician is notified of an event or situation regarding a resident—all of that needs to be neatly, accurately, and thoroughly documented, along with staff schedules, with the census calculated to make sure that the staffing level is in accordance with state laws, so that allegations can be rebutted with proof, he says.
When a facility has that kind of proof, “those claims are more defensible,” says O’Neal.
3. Protect the facility from testimony by ex-employees.
Another element that often crops up in litigation involving long term care organizations is testimony from ex-employees, says O’Neal. “Disgruntled ex-employees will testify that the facility was understaffed, and that the facility knew about the understaffing and didn’t do anything about it, and put the residents at an increased risk of harm.” Even unsubstantiated testimony by ex-employees will be taken as evidence in court, he says. “Ex-employees would say that ‘we were understaffed because I felt that we were understaffed’ without providing any documentation to prove the assertion,” and that may well be taken as evidence of actual understaffing, he says.
Value Of Exit Interviews
Providers can take steps to protect themselves, says O’Neal. The most important thing they can do, aside from keeping accurate and thorough documentation, is conduct detailed exit interviews.
These interviews, which should be thoroughly documented, are aimed at determining why an individual is leaving and give them a chance to tell the provider their side of the story. Then, if the provider sees that person in court giving false testimony, the provider has documentation to show that the real reason the person left was something other than what they’re testifying to, or to prove that they did have a chance to air their grievances. Exit interviews are “aimed at deflating the testimony of someone who may have an axe to grind,” says O’Neal.
4. Use alternative dispute resolution agreements.
Another thing that providers can do to protect themselves from excessive jury awards is have an alternative dispute resolution (ADR) agreement. The two main forms of ADR are arbitration and mediation. The main difference between the two is that the parties in a dispute aren’t bound by what a mediator agrees, whereas with an arbitrator they are.
Increasingly, companies are looking at using both forms—first mediation and then arbitration, says Chris Puri, a partner of Bradley Arant Boult Cummings in Nashville, Tenn., and vice chair of AHCA’s Legal Committee.
Arbitration, the most common form of ADR, benefits both the resident and the provider in the event of a dispute, according to Aon Global Risk Consulting based in Columbia, Md. It benefits the resident because it’s a much faster process and the resident receives financial compensation much more quickly, which may be of critical importance to a resident in his or her twilight years. Another benefit is it greatly reduces transaction costs, which may enable residents and their families to keep more of the settlement than they would have with a lawsuit.
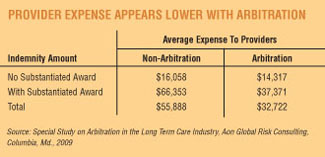
Arbitration agreements benefit providers because the total cost of an arbitrated settlement tends to be about 37 percent lower than a litigated award, according to a 2009 report by Aon Global Risk Consulting.
Make Agreements Fair
The most important thing when drawing up an arbitration agreement is to be fair to both the resident and the provider, says Puri. If it’s not balanced, it won’t be upheld if challenged in court.
Second, keep state law in mind when putting it together. For example, an arbitration agreement that caps any settlement at a certain dollar amount won’t be seen favorably in court if the state doesn’t have the same cap on awards, says Puri.
And make sure the agreement is written in plain language, not legalese. The agreement should be very readable and understandable. For example, “courts have found that the agreement should make it very clear that [the resident] is waiving the right to a jury trial,” says Puri.
Agreements should provide the resident with a period of time after signing it, called a rescission period, that they can change their minds and have the agreement shredded—at least 15 days, but more commonly 30 days.
Finally, the agreement should state that it is under the Federal Arbitration Act (FAA), rather than a state arbitration act, says Puri. “Essentially, the FAA says that states and state courts have to treat arbitration agreements the same way they would any other contract in terms of enforcing it,” Puri explains.
“The reason the FAA was actually passed at all was the notion that state courts had a long-standing hostility toward the use of arbitration,” he says. If the agreement is under the FAA, “the only basis on which you cannot enforce a contract for arbitration would be the same as for any other contract—for example, fraud,” Puri says.
“Those are all things that help [get the provider] to the ultimate goal, and that is to have the agreement be enforceable,” says Puri.
Ensure Agreements Are Enforceable
It’s important that any ADR agreement be enforceable, because according to the Aon study on arbitration, about 12 percent of claims with ADR agreements do not hold up in court, and when that happens the settlement has a much higher total cost. In fact, “the average indemnity amount [awarded] for claims where ADR was challenged and found unenforceable was more than double any other category,” including claims where the case went to trial, the study says.
The most common challenge to an ADR agreement involves the authority and capacity of the person who signed it, so determining whether a resident is truly capable of making that decision is key.
Leave Agent Spot Open
One other thing that Puri personally thinks is a good idea is to leave open who is going to arbitrate the agreement. This would allow the parties to agree on an appropriate arbiter when a dispute arises, perhaps through mediation, with a default course of action identified in case the two are unable to agree, such as having a court appoint an arbiter. The reason for this is that the person or entity that is named in the original agreement may not be arbitrating contracts anymore, or may be inappropriate given the context.
And remember: An arbitration agreement is “only as good as the people in the facility who present it to the patient and/or their family,” says Puri.
“There have been plenty of cases where they’re not signed by the right person, or not explained or not explained right. So with my clients I suggest they have a training program that goes along with the actual piece of paper to make sure it gets presented correctly,” he says.
“The whole purpose is to design a mechanism where if you have a dispute you can resolve it in a way that reduces the conflict as much as possible. As a facility, you ought to want to be able to explain why you think arbitration has advantages for the resident.” The training program should make sure that the people who will be explaining the contract really understand what’s in the contract and what everything means. “A lot of times they don’t,” he says. “It’s just another piece of paper in a big stack.”
Don’t Panic, But Be Aware
While Reagan and Kiepen don’t think the Skilled Healthcare verdict should cause providers to panic—most of the staffing-level-based cases Hooper, Lundy, and Bookman has handled have either been settled out of court or have been dismissed by a court not willing to get into “this kind of fight”—the firm is seeing a number of copycat lawsuits springing up.
“For any state that has a mathematical nursing ratio, there will be attempts to essentially replicate, under whatever the state’s platform for civil liability might be, the equivalent” of the Skilled Healthcare case, says Reagan.
All a plaintiff’s attorney has to do is go through public health records of nursing facilities for technical violations of state regulations and attempt to plead the case as a class-action lawsuit.
“But the sheer size and proportion of the Skilled Healthcare verdict are an aberrance, rather than a huge, enormous comparable risk that everybody is faced with at this point,” says Reagan.
Kathleen Lourde is a freelance writer based in Manassas, Va.