Global Initiative Takes On Dysphagia Treatment
Providers should take steps to incorporate an updated set of standards for the treatment of people with swallowing disorders.
Brenda Richardson
10/1/2018
 In 2017, the Academy of Nutrition and Dietetics and the American Speech-Language-Hearing Association together announced their support of a new global initiative to standardize diets for the treatment of people who suffer from swallowing disorders.
In 2017, the Academy of Nutrition and Dietetics and the American Speech-Language-Hearing Association together announced their support of a new global initiative to standardize diets for the treatment of people who suffer from swallowing disorders.
The International Dysphagia Diet Standardization Initiative (IDDSI) created global standardized terminology and definitions for texture-modified foods and thickened liquids to improve the safety and care for individuals with dysphagia, a disorder that affects an estimated 560 million people worldwide.
Managing Dysphagia Better
Dysphagia can occur at any time during a person’s life, and the most common causes are related to underlying medical or physical conditions. In severe cases, it can lead to life-threatening chest infection, pneumonia, malnutrition, or dehydration.
One of the most common ways of managing dysphagia is the provision of texture-modified foods and thickened liquids. These foods and drinks are provided to help reduce the risk of choking or having material entering the lungs airway and may be commonly referred to as a dysphagia diet.
Officially published in 2017, IDDSI has developed global standardized terminology and definitions for texture-modified foods and thickened liquids to improve the safety and care of individuals with dysphagia of all ages, in all care settings and all cultures. The goal of IDDSI is to have an international language, so that no matter where one is in the world, as a person with dysphagia, as a caregiver, or as a clinician, one can reliably communicate their needs to find food and liquid textures that are safe to eat or drink.
IDDSI in Long Term Care
More than 3,000 participants from 57 countries provided comment on the draft IDDSI Framework before it was finalized and published.
The IDDSI Framework (See Figure 1) places liquids and foods on a single continuum. There is an overlap at Levels 3 and 4. The overlap zone denotes that texture and flow properties of Liquidized foods (Level 3) are very similar or equivalent to Moderately Thick liquids. Similarly, the texture and properties of Pureed food (Level 4) are very similar or equivalent to Extremely Thick liquids.
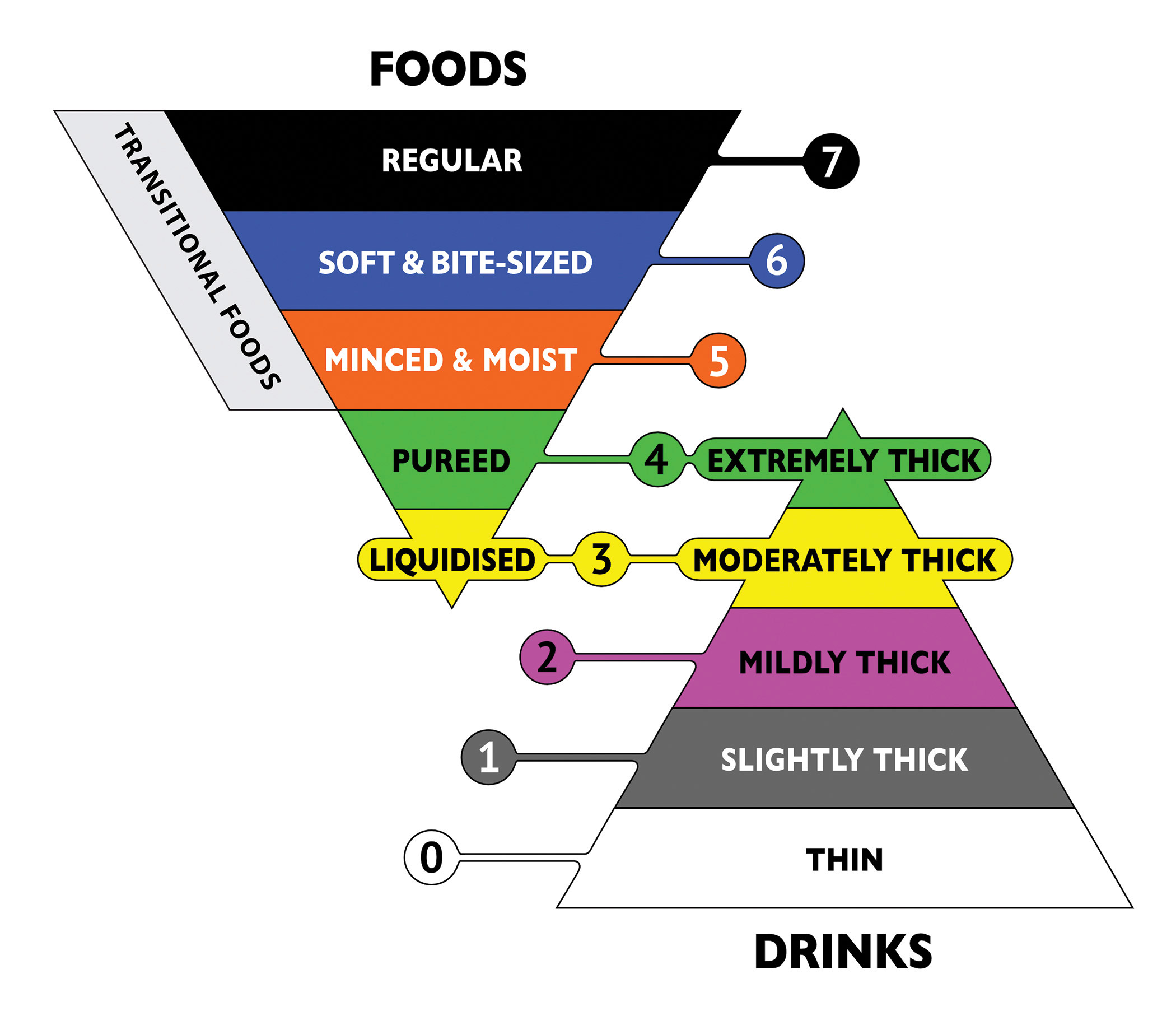
Transitional foods are a group noted on the food side of the pyramid and denote foods commonly used in pediatric treatment or for chewing skill rehabilitation treatment. They are foods that start as one texture, and with moisture or a change in temperature, rapidly change to a different texture that requires minimal chewing (such as potato crisps, wafers, and cheese puffs).
IDDSI has three ways of identifying levels—label, number and color—to enhance communication. IDDSI recommends that at least two of these methods be used to identify IDDSI levels. Specific colors have been chosen to minimize barriers associated with color blindness. It is important to understand that there is no requirement for facilities to provide every IDDSI level.
Testing for All Settings
One of the innovations of the IDDSI Framework is the development of testing methods that can be applied in any setting. The ability to check liquid thickness after adding thickener or checking the actual meal being served to the resident is possible using these testing methods. Particle sizes and texture recommendations for each level have been clearly identified to minimize choking risk.
Forks can be used to assess particle size and food softness, while spoons assist with determining cohesive and adhesive food properties that affect swallowing safety. The testing methods allow for people to check the food on the plate, including the gravy or sauce to be sure that it is the consistency specified by the clinician for safe swallowing.
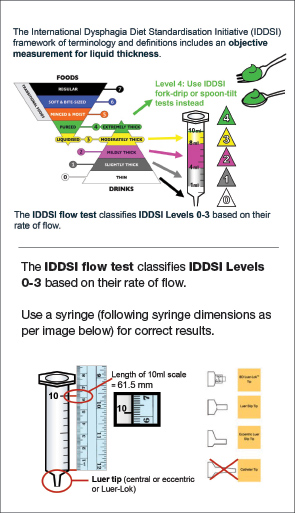
The IDDSI Flow Test allows for liquids to be quickly and easily classified, giving confidence that thick liquids will be consistent from batch to batch of kitchen produced and factory produced items. Further, the IDDSI Flow Test also allows clinicians to determine the thickness of soups, gravies, sauces, and liquid nutritional supplements.
The testing methods and detailed descriptions of each IDDSI level as seen in Figure 2 are available at
www.iddsi.org.
Implementation of IDDSI
Raising global awareness of IDDSI is currently underway, with resources to assist in planning and implementation available from the IDDSI website www.iddsi.org. The food and beverage, thickener, and texture-modified food industries are currently supporting the initiative and developing transitional labels to assist in education regarding the change in terminology.
In the United States, awareness training and education is ongoing, with actual “best practice” implementation planned for 2019.
Some tips for working toward implementation in the long term care facility include:
- Introduce IDDSI to facility management and obtain approval and support;
- Use the www.iddsi.org website resources to educate administrative and clinical staff;
- Determine the IDDSI Levels that will be used in the facility;
- Create a plan of action that includes specific tasks, responsibilities, and time frames;
- Develop policies and procedures;
- Revise diet terminology, diet orders, menus, and recipes;
- Plan staff education/skills/competency training;
- Discuss the changes with the resident council; and
- Educate families and market through newsletters and social media.
Needless to say, implementation of the IDDSI will take collaborative efforts with the registered dietitian nutritionist, speech-language pathologists, certified dietary managers, chefs, dietary staff, nurses, and physicians working together for successful implementation.
The bottom line is that moving toward globally recognized terminology—based on evidence—is critical. As IDDSI says: “Getting it wrong has serious consequences, such as life-threatening chest infection or choking and dying.”
Brenda Richardson, MA, RDN, LD, CD, FAND, is a long term care nutrition expert and president at Brenda Richardson LLC. She can be reached at
Brenda@brendarichardson.com or 812-276-1933.