 Earlier in the days of the COVID-19 pandemic, the Centers for Medicare & Medicaid Services (CMS) issued a March 23 Quality, Safety, and Oversight memo that limited annual state survey activity to focused infection control surveys.
Earlier in the days of the COVID-19 pandemic, the Centers for Medicare & Medicaid Services (CMS) issued a March 23 Quality, Safety, and Oversight memo that limited annual state survey activity to focused infection control surveys.
However, CMS’ latest Aug. 17 directive instructed states to return to the normal survey process as soon as resources in the state allowed and in accordance with states’ COVID-19 reopening plans.
As states move forward in reinstating the original survey process, it is important to prioritize the comprehensive completion of the Facility Wide Resource Assessment (F490).
Be Ready
When state and federal surveyors arrive on site for annual inspections and immediately request multiple pieces of information, the facility should be ready to hand them an organized Facility Assessment binder or PDF version with table of contents containing current, concise, and precise information about the facility’s patient population, resources, and risk assessments.
Per the regulations, the Facility Assessment is beneficial to determine the:
- Appropriate resources to care for residents during day-to-day operations and in emergencies; and
- Specifics consisting of census, facility resident capacity, types of care considering resident population, types of diseases, staff competencies required with emphasis on resident population, cultural aspects, resources (personnel and equipment), services provided (therapy, pharmacy), contracts, memorandums of understanding, and health information technology resources, to name a few.
Think about it this way: The provider is handing the surveyors everything they need to know about the clinical needs of the patient population and the descriptions of what resources are needed to care properly for the residents in that facility.
Specifics Matter
Effort and completion of the Facility Assessment vary across the country. Sometimes, the document is revised once per year. Other times, the document is updated on a regular basis, that is, multiple times within a year. Either way, be sure the content is accurate. Otherwise, surveyors may perceive the entire process with biased impressions that are not in the favor of the facility.
For example, take the patient population section. The patient population is the facility’s resident population, including but not limited to:
- Both the number of residents and the facility’s resident capacity;
- The care required by the resident population considering the types of diseases, conditions, physical and cognitive disabilities, overall acuity, and other pertinent facts that are present within that population;
- The staff competencies that are necessary to provide the level and types of care needed for the resident population;
- The physical environment, equipment, services, and other physical plant considerations that are necessary to care for this population; and
- Any ethnic, cultural, or religious factors that may potentially affect the care provided by the facility, including but not limited to activities and food and nutrition services.
- Some questions to ask about the information in the assessment include:
- How does the facility provide a depiction of the overall clinical and acuity conditions?
- Is it represented in a user-friendly manner?
Population Distribution
It might be helpful to start describing the patient population broadly and then offer more details, like showing the percentage distribution of Resource Utilization Group (RUG) categories for the entire patient population.
Summarizing, the percentage of each RUG category and complementing the table with another visual aid may also significantly help the surveyor gain a rapid understanding of the resident demographic. 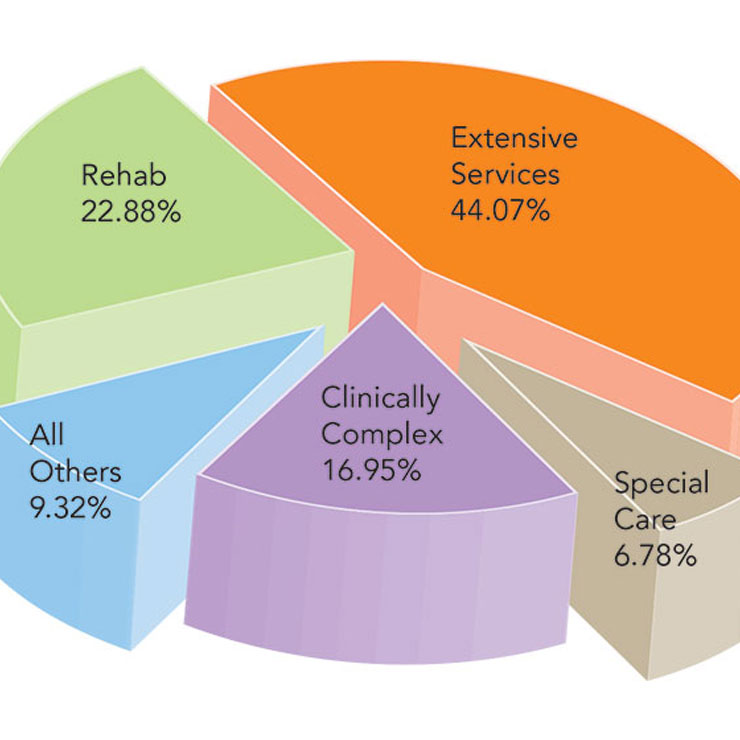
Granted, with the inception of the patient-driven payment model (PDPM), this metric will morph into Case Mix Groups (CMG) over the next few years.
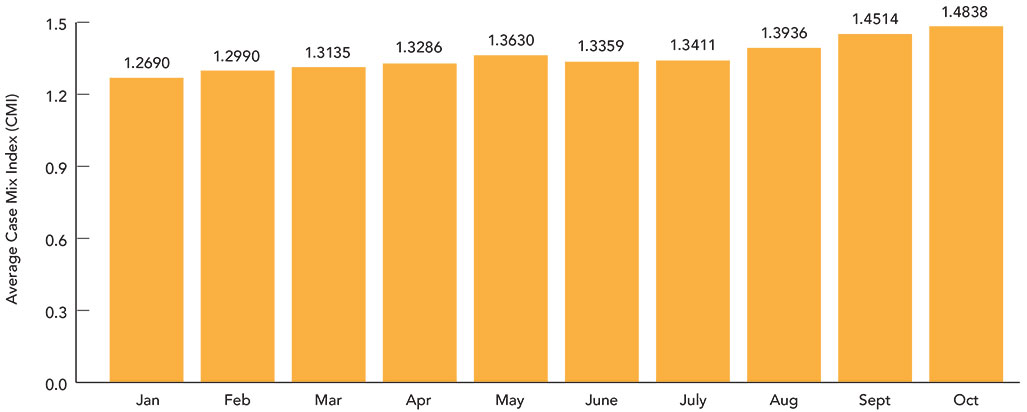
Coupled with the above RUG distribution, the facility should also track and depict the Case Mix Index (CMI). Each RUG level has an assigned CMI.
The graph above portrays the CMI over a period of time.
All Facility Case Mix Index
Each PDPM Case Mix Group (CMG) also has an assigned CMI. The higher the number, the higher the complexity and resources required to care for the resident.
Currently, the different insurance payers use different systems, that is, different CMI systems. PDPM CMG is used for Medicare Part A, and RUG Levels are used for Medicaid case mix levels in certain states.
So, when trying to portray the entire facility acuity, providers need to convert the acuity level to one system for all patients.
Next, consider resources, which include:
- All buildings and/or other physical structures and vehicles;
- Equipment (medical and nonmedical);
- Services provided, such as physical therapy, pharmacy, and specific rehabilitation therapies;
- All personnel, including managers, staff (both employees and those who provide services under contract), and volunteers, as well as their education and/or training and any competencies related to resident care;
- Contracts, memorandums of understanding, or other agreements with third parties to provide services or equipment to the facility during both normal operations and emergencies; and
- Health information technology resources, such as systems for electronically managing patient records and electronically sharing information with other organizations.
The Payroll-Based Journal (PBJ) Five-Star Staffing Domain says a lot about the facility. A score lower than four stars creates the impression to the surveyors that the facility is understaffed, when in fact a low PBJ Domain star rating may be a product of:
- Late transmission;
- Missed transmission;
- Incorrect transmission;
- Data errors; or
- Noncompliance with the PBJ Audit Requests, to name a few.
Be sure to properly show the staffing pattern and schedules by unit. Then, it is critical to ensure that the PBJ submission is currently reported and reflected in existing staffing.
In closing, at a minimum, the Facility Assessment requires revisions on an annual basis. However, best practices include ongoing refinements and updates to the document to properly define the patient population and staffing. Obviously, adjustments are necessary in situations in which the facility encounters significant changes in census or services (such as COVID-19).
Harmony Healthcare International highlights the importance of continued Facility Assessment revisions given the direct impact the content has on the survey process. The more accurate the information, the easier it is for surveyors to understand the services provided and perform an appropriate assessment of the quality of care rendered in the facility.
Kris Mastrangelo, OTR/L, LNHA, MBA, is chief executive officer and president of Harmony Healthcare International. She can be reached at Kmastrangelo@harmony-health care.com.