On October 1, 2019, the Medicare Part A skilled nursing facility (SNF) prospective payment system (PPS) transitioned to the Patient Driven Payment Model (PDPM). PDPM is a case-mix model that relies on the accurate assessment and coding of over 150 items on the SNF minimum data set (MDS) patient assessment instrument. Additionally, many of the patient characteristics and care needs identified by these data elements are used for care planning, various quality measures, and are being considered for incorporation into the SNF value-based payment program.
The Centers for Medicare and Medicaid Services (CMS) has described PDPM as a marked improvement over the prior Resource Utilization Groups, Version 4 (RUG-IV) payment model for the following reasons1:
- Improved payment accuracy and appropriateness by focusing on the patient, rather than the volume of services provided, particularly the rehabilitation therapies.
- Significantly reduced administrative burden on providers by reducing the volume of assessments.
- Re-allocated SNF payments to underserved beneficiaries without increasing total Medicare payments.
In this article we discuss three questions related to the responsiveness of PDPM to adjust payments related to care needs, whether PDPM was calibrated appropriately, and whether provider adjustments in therapy services have impacted outcomes.
Is PDPM responsive to different patient care needs?
It appears so. From day one of PDPM implementation providers were more attentive to the comprehensive assessment and coding of those clinical characteristics and care needs that impact the cost of care. By separately determining payments for each of five case-mix-adjusted components (physical therapy (PT), occupational therapy (OT), speech-language pathology (SLP), nursing, and non-therapy ancillary (NTA) services), the model adjusts payment rates to differences in care needs. Although the PDPM payment model was designed before the COVID-19 pandemic, and any additional costs necessary to provide the more intensive care needed for COVID-19 patients were not contemplated, PDPM generally performed as intended and was able to differentiate many of the cost of care differences between COVID and non-COVID patients.
An AHCA analysis of SNF PPS 5-day assessments depicted in Fig. 1 highlights significant differences in PDPM Nursing component case-mix index (CMI) rate multipliers for urban provider patients with a primary reason for SNF stay diagnosis of COVID-19 versus all other admission diagnoses between April 2000 and July 2021. Generally, COVID-19 patient CMIs were 0.3 to 0.5 points higher than non-COVID patients. With an unadjusted urban federal rate of $108.16 in fiscal year (FY) 2021, this translated to about an additional $32.44 to $54.08 per day per COVID patient within just the Nursing component.
Fig. 1. PDPM Nursing Component CMI Trends – Urban Providers - COVID vs. Non-COVID Primary Diagnosis2
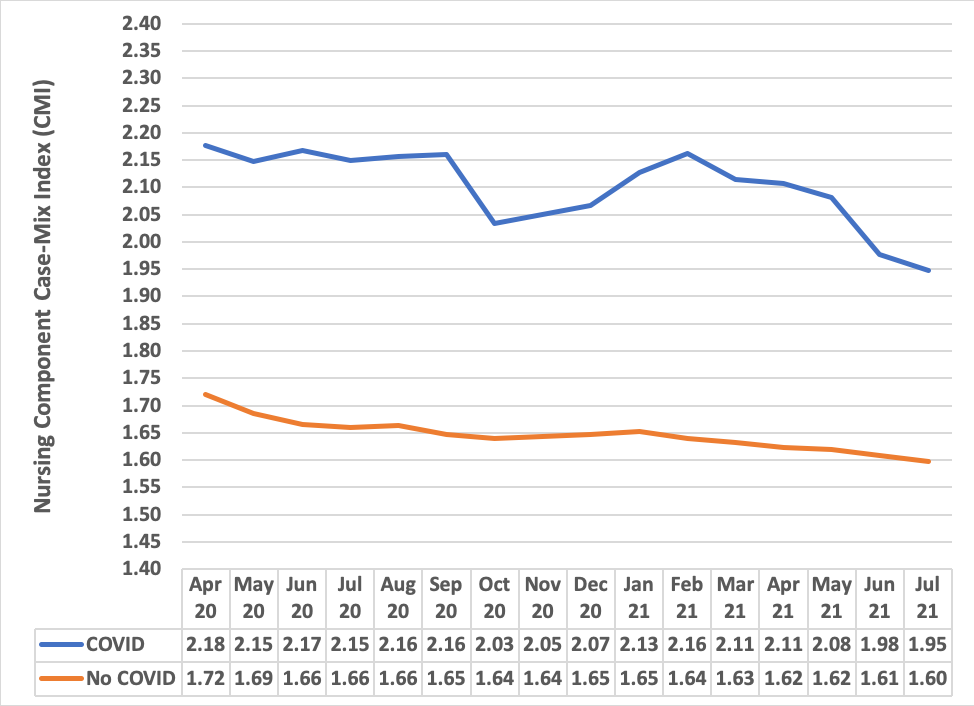
Similar patterns were observed for the SLP and NTA components while the opposite pattern occurred with the PT and OT components. This makes sense because the Nursing, SLP, and NTA component CMIs are influenced primarily by more complex medical conditions and specialized service needs while the PT and OT component CMIs are weighted more towards post-surgical conditions and function level. With COVID-19 being mapped to a lower level PDPM Medical Management condition group, and infection control measures including isolation restricting a patient’s ability to move about, it is not surprising that the PT and OT component CMIs for COVID-19 patients trended lower during COVID-19 surges.
Overall, the shifting of month-to-month average CMIs for all components consistent with COVID-19 surges indicates that PDPM is responsive to patient care needs. However, further analysis is needed to determine whether PDPM adequately captures all care costs associated with a COVID-19 diagnosis.
Was PDPM accurately calibrated in a budget-neutral manner?
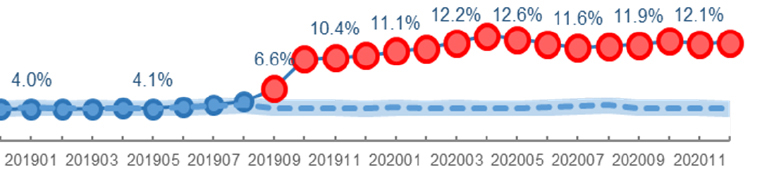
Perhaps not. While more responsive to adjusting payments to reflect different care needs than the prior RUG-IV payment model, CMS did not factor in possible changes in MDS coding patterns once additional MDS items impacting case-mix rates were added to the PDPM rate calculation approach. For example, as depicted in Fig. 2, CMS notes that prior to the PDPM implementation, only about four percent of Medicare patients were coded with having depression on admission, while this number rose to double digits beginning October 2019 and remained stable even as the COVID-19 pandemic hit. The MDS items D0300 and D0600 reflecting the presence of depression can by themselves impact the PDPM Nursing component unadjusted federal rate from $16.43 to $44.90 per day.
Whether such coding changes reflect more accurate coding will ultimately be determined through Medicare audits. However, given that recent CMS Chronic Conditions Warehouse SNF provider public use files for 2019 indicates that 54 percent of SNF Medicare admissions have a history of depression3, the increased reporting of depression may reflect improvements in assessment that can translate to improved care planning related to the mood disorder.
Fig. 2. Percentage of SNF Stays Coded with Depression1
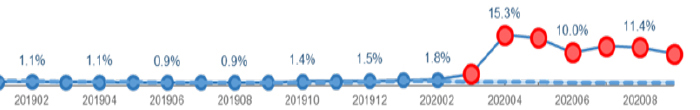
In contrast, other items MDS items impacting payments only showed a change with the onset of the COVID-19 pandemic consistent with a highly infectious disease. Beginning April 2020, the reporting of MDS item O0100M2 reflecting isolation or quarantine for active infectious disease skyrocketed from less than two percent to over 15 percent and remained in double-digits (Fig. 3). In other cases, the coding for some MDS items changed upon PDPM implementation and then changed again with the onset of COVID-19.
Fig. 3. Percentage of SNF Stays Coded with Isolation1
Since the patient population did not change with PDPM, only the payment model, CMS is considering adjusting the payment model to account for the observed coding patterns that differ from what was anticipated so that total Medicare payments under PDPM are equivalent to what would have been paid under RUG-IV. However, teasing out the impact of unanticipated COVID-19 factors from PDPM-specific factors during a still-ongoing pandemic is challenging, and any recalibration overcorrection could be problematic.
In the FY 2022 SNF PPS proposed rule4 and final rule5 CMS suggested a conceptual approach to account for the impact of the COVID-19 by analyzing SNF Part A stays without a COVID-19 diagnosis or use of the 3-day qualifying hospital stay (QHS) or benefit period waivers as indicated by a DR condition code on the SNF claim. As depicted in the Expected CMI column in Table 1, CMS estimated what the average component CMI would be under PDPM if no coding pattern changes occurred upon implementation.
However, the Actual FY 2020 average CMI for the SLP, Nursing, and NTA components for patients without COVID and that did not access SNF care via the COVID-19 waivers were higher than expected, which resulted CMS estimating that payments were 5 percent more than expected.
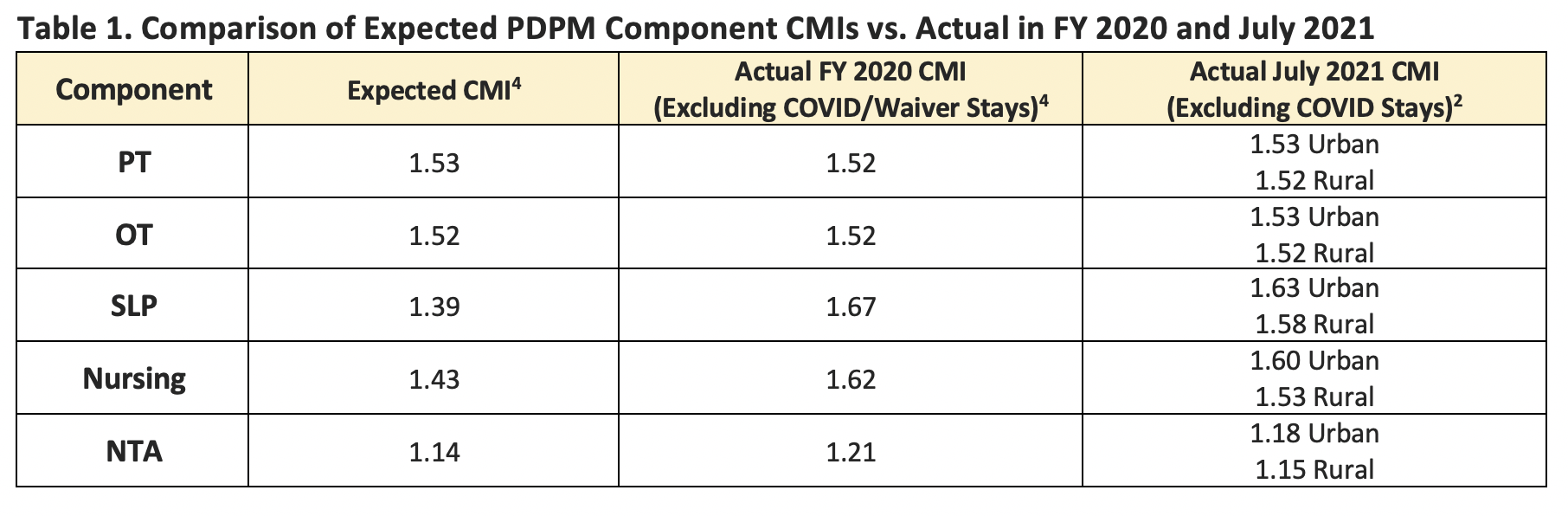
CMS proposed a “parity adjustment” to the component base rates to recalibrate payments to be budget neutral. In response to public comments related to using skewed COVID-era data to estimate a parity adjustment, in the final rule CMS deferred any decisions in order “…to refine the data we have collected in developing a proposed methodology that will be included in the FY 2023 SNF PPS Proposed Rule.” More current MDS data suggests that this was the right decision. As demonstrated in the last column of Table 1, AHCA analysis of the Urban and Rural average PDPM SLP, Nursing and NTA component CMIs of non-COVID patients during July 2021 were lower than the FY 2000 average CMIs. This is significant as July 2021 was a period before the onset of the Delta and Omicron COVID-19 variants when most SNF residents were vaccinated and the infection rates in SNFs were at their lowest levels since the pandemic started. This indicates that there does appear to be some “spillover” impact of the COVID-19 pandemic on non-covid patient CMIs’ that is exacerbated during surges that needs further evaluation prior to finalizing any proposed parity adjustment.
Did providers “right size” therapy service delivery as intended by CMS?
Early indicators suggest yes. While providers changed therapy service delivery patterns upon implementation of PDPM there were no noticeable differences in patient outcomes related to therapy service delivery. As stated above, one of the motivators and goals of CMS for PDPM was to shift the incentives of the payment model from the volume of therapy services provided to providing the amount of therapy based on patient need. CMS anticipated reductions in therapy minutes as providers would no longer be incentivized to furnish just enough therapy to achieve the various RUG-IV case mix payment thresholds, particularly the 720-minute Ultra-High and 500-minute Very-High rehab groups.
In the FY 2022 SNF PPS final rule5 CMS indicated that the amount of therapy minutes during the 5-day assessment decreased from 91 minutes to 62 minutes per day. Additionally, patients receiving any concurrent or group therapy during part of a stay increased from one to about 30 percent in the months leading up to the pandemic, while nearly all patients returned to individualized therapies for infection control purposes upon the first wave of the COVID-19 pandemic. A recent qualitative survey suggests that therapy services also shifted significantly to bedside care6.Overall, most therapy continues to be delivered one-on-one. AHCA noted this in submitted comments to CMS describing quarterly trends, “…the SLP peak average percentage of the use of concurrent and or group therapy minutes per stay in FY 2020 was 2.35 percent, for PT it was 5.62 percent, and for OT it was 5.59 percent.”7
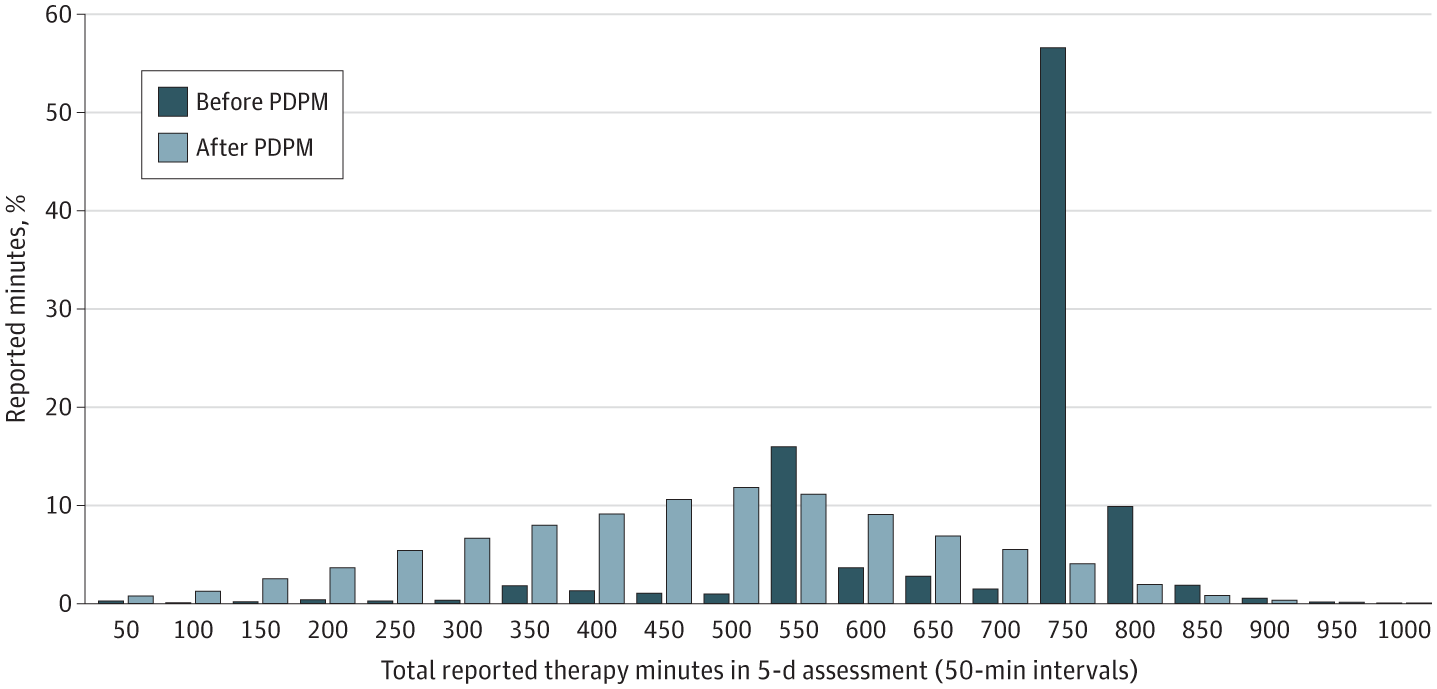
With regards to the payment thresholds, a CMS official reported that, as was intended, therapy service delivery reflects a normal distribution in reported therapy minutes rather than the previously observed spikes at 500 and 720 minutes1. As depicted in Fig. 4., researchers analyzing SNF data for patients with a hip fracture diagnosis prior to and for the first six months of PDPM observed a similar normalization of therapy minutes reported on the 5-day assessment away from spikes at the previous RUG-IV thresholds.
Fig. 4. Distribution of Therapy Minutes Provided as Reported in 5-Day Scheduled Assessment for Patients With Hip Fracture Diagnosis Before and After the Patient Driven Payment Model (PDPM)8
Regarding patient outcomes, CMS has indicated they are closely monitoring whether any changes in therapy service delivery are having detrimental impacts on patient outcomes. In the FY 2022 SNF PPS final rule, CMS stated “…we observed no significant changes in the percentage of stays with falls with major injury, the percentage of stays ending with Stage 2–4 or unstageable pressure ulcers or deep tissue injury, the percentage of stays readmitted to an inpatient hospital setting within 30 days of SNF discharge, or other similar metrics.”5
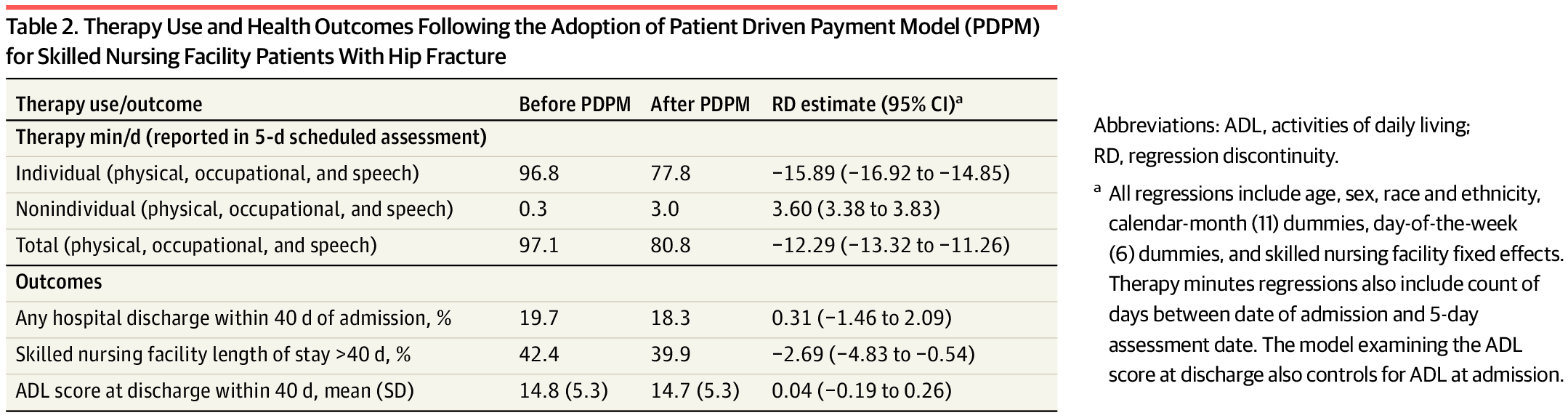
As depicted in Table 28, researchers analyzing SNF data for patients with a hip fracture diagnosis prior to and for the first six months of PDPM reported similar findings that changes in therapy service delivery patterns under PDPM (minutes and individual vs nonindividual) did not impact outcomes related to hospital readmissions, length of stay, and functional score at discharge parameters investigated.
Additional outcomes analyses may be necessary to identify best practices for “right sizing” therapy service delivery, however, these preliminary findings suggest that the CMS intent for the payment model to incentivize person-centered care and to provide services based on the “clinical judgment” of the therapy clinician appears to be occurring.
Part II is now available.
1 Kane, John, Patient Driven Payment Model: Understanding the Impacts. 72nd AHCA/NCAL Convention & Expo. October 11, 2021.
2 AHCA Analysis of CMS SNF PPS 5-Day Assessments.
3 Skilled Nursing Facility by Provider and Service Table 2019. Data.CMS.Gov.
4 86 FR19954, April 15, 2021. Medicare Program; Prospective Payment System and Consolidated Billing for Skilled Nursing Facilities; Updates to the Quality Reporting Program and Value-Based Purchasing Program for Federal Fiscal Year 2022. Proposed Rule.
5 86 FR42424, August 4, 2021. Medicare Program; Prospective Payment System and Consolidated Billing for Skilled Nursing Facilities; Updates to the Quality Reporting Program and Value-Based Purchasing Program for Federal Fiscal Year 2022; and Technical Correction to Long-Term Care Facilities Physical Environment Requirements. Final Rule.
6 Reddy, A, et al. Rapid changes in the provision of rehabilitation care in post-acute and long-term care settings during the COVID-19 pandemic. JAMDA. 2021, Nov;22(11):2240-2244.
7 AHCA submitted comments re. FY 2022 SNF PPS Proposed Rule. CMS–1746–P.
8 Rahman, M, et al. Association between the patient driven payment model and therapy utilization and patient outcomes in US skilled nursing facilities. JAMA Health Forum. 2022.3(1).e214366.