 In December 2023, the Office of the Assistant Secretary for Planning and Evaluation (ASPE) at the U.S. Department of Health and Human Services announced the publication of a report prepared by RTI International that discusses the adoption of electronic health records (EHRs) and interoperable health information technology (HIT) in nonhospital and nonphysician health care settings, including nursing facilities and some assisted living residences. This study can help providers and policymakers understand and overcome technology gaps that have resulted from long term and post-acute care (LTPAC) providers being excluded from federal funding under the Health Information Technology for Economic and Clinical Health Act.
In December 2023, the Office of the Assistant Secretary for Planning and Evaluation (ASPE) at the U.S. Department of Health and Human Services announced the publication of a report prepared by RTI International that discusses the adoption of electronic health records (EHRs) and interoperable health information technology (HIT) in nonhospital and nonphysician health care settings, including nursing facilities and some assisted living residences. This study can help providers and policymakers understand and overcome technology gaps that have resulted from long term and post-acute care (LTPAC) providers being excluded from federal funding under the Health Information Technology for Economic and Clinical Health Act.
The report, titled Health Information Technology Adoption and Utilization in Long-Term and Post-Acute Care Settings, is based on an environmental scan of the literature, as well as interviews with providers and subject matter experts. Researchers found that LTPAC providers have organically adopted EHRs to support clinical and business needs. However, interoperable exchange of health information (meaning information is sent, received, and understood between computer systems), is not routine or widely used.
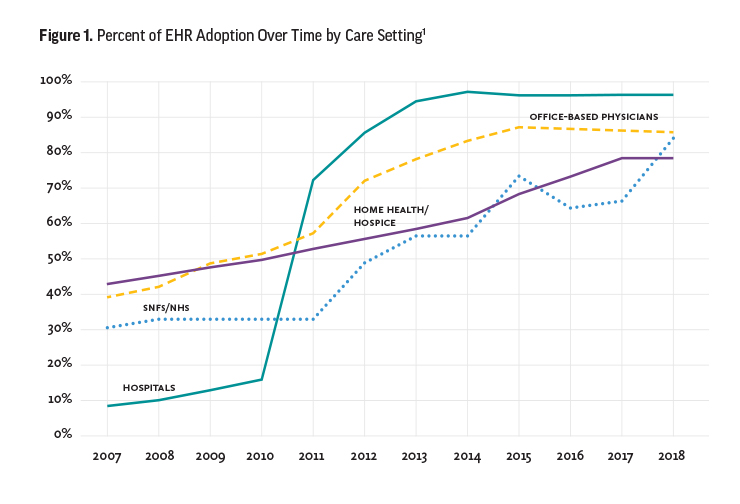
Pertinent to American Health Care Association/National Center for Assisted Living (AHCA/NCAL) member interests, the study reports EHR adoption rates as follows: “Yet despite the lack of a federally funded program and policy requirements, estimates of EHR adoption rates among nursing home and [skilled nursing facility] providers, as well as [home health agencies], were greater than 78% in 2018, which is on par with EHR adoption in office-based primary care settings. Residential care settings were estimated to be much lower overall, at 26%—higher than that for larger facilities and much lower for small facilities.”
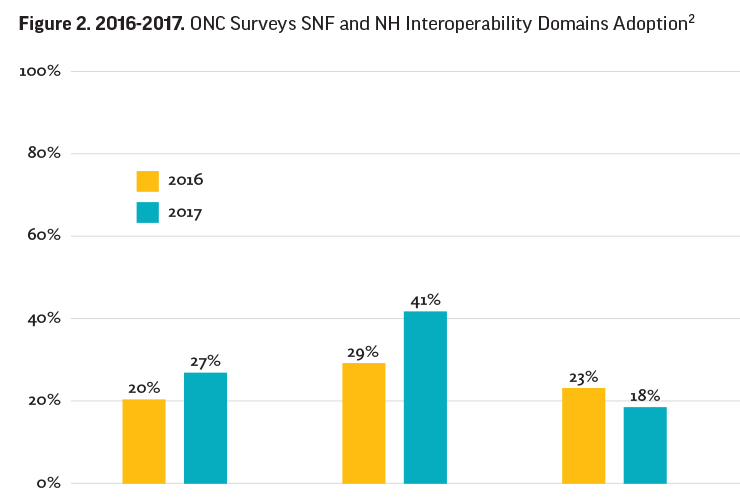
While LTPAC providers utilize EHRs, modernization using this technology to exchange information with external entities remains slow without focused policy levers. The RTI report highlights findings from an Office of the National Coordinator for Healthcare Technology (ONC) survey that skilled nursing facility (SNF) and nursing home (NH) providers’ application of three interoperability domains lags well behind EHR use.
These are the three interoperability domains:
1. Find. Do you or your staff electronically search for or query your patients’ health information from sources outside your facility?
2. Send. Do staff at your SNF electronically send key clinical information, such as labs, medications, or problem lists, to outside organizations on a routine basis (excluding fax, e-fax, or minimum data set)?
3. Integrate. Is staff easily able to integrate patient health information that you electronically receive into your
EHR without manual entry or scanning? (see Figure 2 for SNF and NH interoperability domain rates).
There is increasing pressure from consumers and policymakers for LTPAC providers to increase interoperable HIT technology sooner rather than later. The report’s lead author, Michelle Dougherty, MA, RHIA, from RTI International, noted, “Expectations are growing that you have and share information electronically and interoperably. Increasingly, LTPAC providers will face pressures to use health IT in more sophisticated ways to support clinical care and reduce administrative burden, maintain partnerships with referral sources, electronically report required information, and plan for the emerging value-based care models. Advanced technology is used by your residents and their families, your workforce, your care partners, and your payers.”
However, the RTI study highlighted numerous structural, regulatory, and financial barriers that have inhibited the adoption and use of interoperable HIT in LTPAC settings despite the potential advantages associated with efficiencies and care coordination that can lead to better clinical outcomes.
The six overall study findings are as follows:
- LTPAC providers are adopting EHRs to support their clinical and business needs (80 percent for nursing homes and home health), but interoperable exchange of health information is not routine or widely used.
- Data from LTPAC organizations is needed by others, but LTPAC providers lack monetary incentives, policy requirements, or a strong business case to increase interoperability.
- LTPAC use of interoperability features available in their EHRs lags without a driver or policy lever.
- Many LTPAC providers struggle to prioritize EHR optimization, and few have available resources for training and workflow changes.
- Innovators in LTPAC HIT are focusing on telehealth, remote patient monitoring, medication management, functional assessment and activity monitoring, shared care planning, social connectedness and engagement, safety, and data analytics.
- There are opportunities for emerging policies to support interoperability in LTPAC.
The report’s findings align with ongoing AHCA/NCAL’s efforts to advance policies and funding opportunities for our membership to increase the prevalence of interoperable health information exchange to improve care and reduce costs.
One of these activities is AHCA/NCAL’s participation in the LTPAC Health IT Collaborative, which is a public-private group of stakeholder organizations advocating meaningful, effective, and accessible health information and technology policies, strategies, standards, resources, products, and services. These technologies enhance the delivery of coordinated, quality care for people with chronic and/or complex needs. The Collaborative was formed in 2005 to advance health IT issues by encouraging coordination among national associations representing clinicians, providers, information technology developers, researchers, and others with specific expertise in LTPAC. Visit the Collaborative website at ltpachit.org for more information.
Another group AHCA/NCAL is involved with advocates the advancement of inter-operable HIT with nursing facilities: the Moving Forward Nursing Home Quality Coalition (movingforwardcoalition.org). This coalition was spurred by the publication in 2022 of The National Imperative to Improve Nursing Home Quality, a consensus report by the National Academies of Sciences, Engineering, and Medicine (NASEM).
The Moving Forward Coalition is seeking input across a broad spectrum of stakeholders to develop short- and long-term approaches to operationalize recommendations from the following five HIT strategies to improve nursing home quality, proposed in the NASEM report:
- Identify pathways to provide financial incentives to nursing homes for certified EHR adoption.
- Develop and report measures of HIT adoption and interoperability.
- Measure and report nursing home staff, resident, and family perceptions of HIT usability.
- Develop and implement training in core HIT competencies for nursing home leadership and staff.
- Evaluate studies of HIT use, disparities in HIT adoption and use, innovative HIT applications, and assessment of perceptions of HIT usability.
While there are several challenges for nursing facility and assisted living organizations to adopt and implement interoperable HIT universally, many providers have been able to successfully implement such technology into their clinical and administrative workflows today. Many of these successes resulted from strategic incremental enhancements of interoperable technology functionality with key hospitals, physicians, therapy providers, labs, pharmacies, and other care partners, rather than from sweeping disruptions to ongoing workflows.
The ASPE report developed by RTI discusses success stories in which LTPAC providers that have “champions” who see the value in using interoperable technologies, such as EHRs, remote patient monitoring, and telehealth, were able to improve efficiencies and clinical outcomes and grow the programs organically within each organization. As Dougherty emphasized, “Every LTPAC organization should have a core team who is responsible for planning and deploying health IT based on your clinical and business needs and is keeping up on the importance of interoperability and the impact it will have on your operations and growth. Important efforts are happening in your state and national associations—stay engaged, attend training, and participate in opportunities that increase your interoperability footprint.”
Daniel Ciolek is associate vice president, therapy advocacy, for the American Health Care Association.
References
1. Excerpt from Health Information Technology Adoption and Utilization in Long-Term and Post-Acute Care Settings. RTI International. December 2023, Exhibit 2.
2. Excerpt from Health Information Technology Adoption and Utilization in Long-Term and Post-Acute Care Settings. RTI International. December 2023, Exhibit 3.