Pressure ulcers are a devastating life safety issue impacting individuals when their health may be very vulnerable. They are associated with increased cost, pain, infection, and death. Residents in long term care facilities often present with varying health conditions that put them at an increased risk for the development of pressure ulcers.
Also known as pressure sores, bedsores, and decubitus ulcers, a pressure ulcer is defined as “localized injury to the skin and/or underlying tissue, usually over a bony prominence as a result of pressure or pressure in combination with shear” by the National Pressure Ulcer Advisory Panel.
An estimated 2.5 million pressure ulcers are treated annually at a staggering cost.
The financial impact of treating pressure ulcers is significant, as the cost associated with the treatment of a full-thickness wound can be as much as $70,000. The projected cost in the United States for treating pressure ulcers is $11 billion per year, according to M. Reddy, S.S. Gill, and P.A. Rockon, reported in the Journal of the American Medical Association.
Patient Trauma High
While treatment cost is a major concern, it is overwhelmed by the impact of this demoralizing safety issue on the patient. The presence of a pressure ulcer imposes many physical restrictions and lifestyle changes.
The incidence rate demonstrates the impact that pressure ulcer events place not only on the patient but the health care system. The incidence of pressure ulcers in the long term care setting ranges from 2.2 percent to 23.97 percent, according to J. Maklebust in Nursing Clinics of North America (see theclinics.com). People with impaired mobility, such as those with stroke, spinal cord injury, or cognitive impairment, are at risk for the development of pressure ulcers.
Diabetes mellitus, end-stage renal disease, and thyroid disease also predispose individuals to the development of pressure ulcers.
A risk assessment should be completed to identify individuals who may be at risk. A reliable tool utilized to predict individuals at risk for the development of pressure ulcers is the Braden scale.
Evidence-based guidelines for the prevention and treatment of pressure ulcers are available and easily obtainable. With so much information and knowledge at hand, why do care providers fail to implement these protocols in practice? In long term care, the literature reveals that nurses may be aware of best practices and still not utilize them. It is critical that nursing facilities implement educational programs and evidence-based guidelines to prevent and treat pressure ulcers.
What is also important is the implementation of training in core competencies for all levels of nursing staff, including registered nurses, licensed practical nurses, and certified nurse assistants.
A Case Study
The decision was made to review a long term care facility whose pressure ulcer incident rate was 21 percent and determine what best practices could be implemented to reduce it. The aims identified for the project were to increase staff knowledge of evidence-based intervention for skin care and prevention of pressure ulcers and decrease the incidence of institutionally acquired pressure ulcers and decrease the severity of ulcers in residents who reside in long term care centers.
To increase staff knowledge and to develop the evidence-based pressure ulcer and treatment protocols, the project team conducted a systematic review of existing literature.
After completing the review, the first phase of the project examined whether a sample of nurses’ knowledge would increase after receiving training on preventing pressure ulcers. The methodology entailed implementation of a knowledge pre-test, provision of a curriculum, and implementation of a post-test with 46 employees at the facility. The desired outcome was that the intervention group would have better scores on a post-test, compared with pre-test scores, after receiving education based on learning objectives.
The second phase of the project examined whether implementing an evidence-based pressure ulcer prevention protocol could decrease the incidence of pressure ulcers among a sample of patients. The second phase also looked at the implementation of an evidence-based wound treatment protocol to improve upon the severity of pressure ulcers that already existed.
The Results
After receiving extensive training on preventing pressure ulcers, the 46 participants’ knowledge of pressure ulcers was tested using a 10-item test before the intervention (pre-test) and after the intervention (post-test), which allowed for an assessment of their gain in knowledge over time.
As shown in Figure 1, a review of the results revealed the nurses were able to answer on average, 5.74 questions out of the 10 correctly before training, and were able to answer 8.28 questions correctly after training. The results of a correlated t-test show that the increase in the nurses’ knowledge from pre-test to post-test was statistically significant, t (45) = -9.40, p <. 001.
Data analyzed from a sample of 66 residents of a nursing home included demographics, health risk for developing pressure ulcers, pressure ulcer stage before and after the implementation of the training, and protocols.
The residents’ ages ranged from 50 to 97 years.
The primary outcome variable was whether the residents developed a pressure ulcer after the implementation of evidence-based protocols. No new cases of pressure ulcers emerged among the 61 residents who began the program with no pressure ulcers, suggesting that the prevention program was effective.
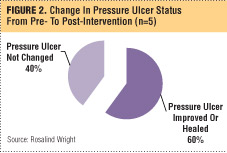
For those residents who had a pressure ulcer prior to the project’s implementation, an evidence-based
protocol on treatment was used to determine if worsening of the pressure ulcer could be prevented. The five residents with existing pressure ulcers started with a treatment program, which was also effective, as the severity of the pressure ulcers did not worsen: Sixty percent of the pressure ulcers improved or healed, and 40 percent remained the same.
In Summary
The project demonstrated that there was a statistically significant change in knowledge from pre-test to post-test. It appears that these gains in knowledge may impact practice. In addition, during the course of this project, with the introduction of education and evidence-based protocols, the incidence of new pressure ulcers was zero, the severity of pressure ulcers decreased, and the overall pressure ulcer incident rate decreased to 3.08 percent.
Although the organization was pleased with the results, the facility was keenly aware of avoidable vs. unavoidable pressure sores and the difficulty in ensuring that knowledge endures and treatment and change in behaviors are sustained. Thus, the training continued for nursing employees, and new protocols were implemented throughout the facility, with the goal of zero tolerance for pressure ulcers. ■
Rosalind Wright, RN-BC, doctor of nursing practice, RAC-CT, CNHA, Fellow, has more than 30 years of leadership experience in long term care, acute care, and academia. Wright serves as vice president of quality management for VMT Long Term Care Management and administrator of Unique Residential Care Center, a 230-bed skilled nursing facility, in Washington, D.C. She successfully administered her facility to a Five-Star nursing home rating from CMS.
Acknowledgement: The author would like to acknowledge the following people for their assistance in this project: Laila Alamgir, MD, medical director; Jacqueline Holmes, director of quality and staff development; and Francise Dyson, executive assistant.