Building a Wound Management Program
A new approach bridges the gap between skilled nursing facilities and outpatient wound clinics.
Roya Agahi
2/1/2018
It is estimated that more than 2.5 million people in the United States develop pressure ulcers each year. Prevalence is widespread in all care settings, with estimates of 10 percent to 18 percent in acute care, 2.3 percent to 28 percent in long term care, and 0 percent to 29 percent in home care. These wounds bring pain, associated risk for serious infection, and increased health care interventions.
Pressure ulcers, also known as pressure injuries, are a leading threat to quality of care. Research by the U.S. Department of Health and Human Services’ Agency for Healthcare Research and Quality shows that pressure ulcers cost the nation’s health care system more than $11 billion a year.
In long term and post-acute care (LT/PAC), a significant number of patients are admitted with existing pressure ulcers that have developed in the community or during their stay at a hospital. Others will have pressure ulcers develop during their skilled nursing facility (SNF) stay due to reasons of clinical comorbidities, lack of mobility, or decline in functional status related to a hospital stay.
This article will review the evolution of wound care and how providers can build a transitional wound management program that will help patients succeed post-discharge.
The Wound Care Evolution
The Patient Protection and Affordable Care Act enacted in 2010, and the Improving Medicare Post-Acute Care Transformation Act of 2014, have had a significant impact on SNFs, mandating that patient care services be focused on quality rather than quantity in order to improve the patient experience and outcome.
As such, SNFs’ wound care has changed accordingly. In recent years, the Centers for Medicare & Medicaid Services (CMS) has developed appropriate measures to monitor and evaluate the quality of pressure ulcer and wound care provided to Medicare and Medicaid beneficiaries in SNFs. In addition, many accountable care organizations follow CMS guidelines to ensure their patients receive appropriate care in SNFs.
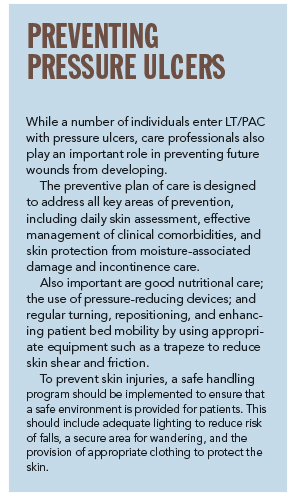
Wound care itself has shifted to focus not only on the plan of care and effective treatment, but also on preventive measures. While pressure ulcer evidence-based policies and competency-driven practice have changed wound care broadly, pressure ulcer comprehensive risk assessment and preventive interventions have become the immediate areas of focus in the plan of care. Pressure ulcer prevention has created a new movement in wound management.
Transitional Wound Management Program
Even though the goal is to heal the wounds during a stay at a SNF, data from Centers Health Care in April 2017 show that around 8.4 percent of patients will be discharged home with wounds due to the status of their chronic wound and patients’ clinical comorbidities. These patients will need to continue to receive wound treatment management in outpatient wound clinics in the community.
In order to make a successful transition from the SNF to the outpatient clinic, the SNF should start as far back as on the first day of the patient’s admission to the SNF. On day one, all necessary information about the patient should be collected and reviewed. Identifying where the patient received her wound care prior to coming to the SNF as well as any documentation that came with her is important to establish from the start. This history can be shared with the outpatient wound clinic early on so they know in advance where the patient started out and that the patient is now receiving rehabilitation services in the SNF.
The transitional wound management program is a partnership between the SNF and the outpatient’s wound clinic. The SNF should set up post-discharge follow-up appointments with the outpatient’s wound clinic and have a “hand-off” with clinicians. This involves providing critical information to the wound clinic such as patient past medical history, description of the wound, progress in the wound healing, treatment agents and procedures that were used in the SNF, and the wound physician involved with the care.
A wound nurse-to-wound nurse hand-off with a progress report is crucial to ensuring the patient’s safety during the transition between settings.
The SNF should follow up with the patient within 48 hours post-discharge to make sure that an appointment with her primary care physician takes place. Additionally, the SNF should set up a post-discharge appointment with the outpatient clinic to get a progress report on the patient’s wound condition. All of these steps reinforce the safety of the patient through the continuum of care.
Investing In Education
Investing in patient and family education will help ensure success beyond the discharge process. A simple guide on preventive pressure injury measures will help family and caregivers manage the patient’s pressure ulcer.
Education involving safe patient handling techniques in order to prevent skin tears is highly important, as well as determining the knowledge and wound care competency of the patient and his or her caregiver. Patient and family education and participation in the plan of care are critical elements to the wound-healing process and will impact positively on wound program outcomes.
If done appropriately, the transitional wound management program can not only bridge the gap between the SNF and outpatient wound clinics, but reinforce the safety of the patient and impact the outcome positively.
Roya Agahi, RN, is chief clinical officer at Centers Health Care, Bronx, N.Y. She can be reached at ragahi@centershealthcare.org.