The challenge is to catch it early, reverse it when possible,
and balance interventions with personal preferences. This requires a
team where everyone is on the same page, communicates effectively, and
has the latest, best tools at their disposal.
The Many Ingredients of Weight Loss
Older adults are generally at risk for weight loss and malnutrition
because of the problems and deficits related to aging—some physical,
some mental or emotional, and others socioeconomic or cultural. All of
these issues can contribute to poor appetite and weight loss and a
cascade of conditions and illnesses.
The cause of weight loss may seem obvious—the person isn’t getting
enough calories and nutrients. However, it is much more complex. This
problem often results from a combination of factors. Among the many
problems that can contribute to weight loss and malnutrition are:
Dementia or other cognitive impairments that cause people to lose their appetite or forget to eat;
Malignancies or other illnesses, such as heart disease, thyroid disease, and infections;
- Depression;
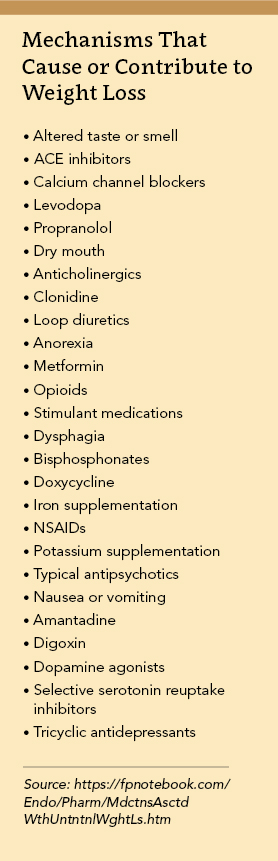
- Certain prescription medications (see table, below);
- Restricted diets;
- Lack of access to preferred foods;
- Limited income;
- Lack of transportation;
- Alcoholism or drug addiction; and
- Dental or oral health pain or problems.
Watch for Red Flags
It is important to note that unplanned weight loss in an elderly
patient should always be a red flag and should lead to some assessment.
“When I get a call from a nurse that a patient has triggered for weight
loss, I have a protocol that I use,” says David Smith, MD, CMD,
president of Geriatric Consultants in Brownwood, Texas. “Tier one
involves some historical questions and observations to uncover any
circumstances that would indicate common reasons for weight loss or
reasons that are uncommon but easy to identify—such as dental problems
or other oral issues, distorted body image, or dissatisfaction with the
food being served.”
Tier two of Smith’s protocol looks for issues that are a bit more
uncommon and are more expensive to evaluate, such as the presence of
swallowing problems or metabolic disease. If the cause is still
undetermined after tier one and two assessments, Smith goes to tier
three, which involves more invasive and costly assessments designed to
uncover issues such as a malignancy.

“People often jump to ‘cancer’ as a likely medical cause for weight
loss. In truth, there are many other more likely culprits—from heart
failure and thyroid issues to infections and depression,” says T. S.
Dharmarajan, MD, MACP, FRCP(E), AGSF, vice chair of the Department of
Medicine and clinical director of the Division of Geriatrics at
Montefiore Medical Center (Wakefield Campus) in Bronx, New York.
“If you encounter weight loss, you need to identify the root causes
as quickly as possible, and not make assumptions or leap to
conclusions,” says J. Kenneth Brubaker, MD, CMD, medical director of
Masonic Village in Elizabethtown, Pa. Start with the “low-hanging
fruit,” he suggests, such as drugs that may be causing or contributing
to weight loss, or the patient simply doesn’t like the food being
served.
Dharmarajan agrees, noting, “Sometimes if you just ask, you will
find out that it’s something fixable such as they can’t cut or chew the
steak, or they don’t like fish.”
Finding out why someone isn’t eating requires a bit of detective
work, Dharmarajan says. The person’s plate is one important clue. “Look
at the patient’s tray after he or she eats. You can see what and how
much they’re eating,” he says.
While drugs that help depression can lead to improved appetite,
Smith says that several nonpsychiatric drugs—such as clonidine,
digitalis, levodopa, prazocin, reserpine, amiodarone, and
steroids—actually can cause depression and negatively impact appetite
and eating.
Even if there is a medical problem, it can be fixed fairly easily.
For instance, Dharmarajan says, “I had a new resident who told me that
she had no appetite for anything. I asked her simply, ‘Do you miss your
grandchildren?’ She started crying. I put her on antidepressants, and
within a few weeks, she was eating again. Her daughter thanked me for
giving her ‘mom back’ to her.”
When Patients Live Alone, Nutrition May Suffer
Particularly when older people live independently—either in the
community or senior housing where they have their own apartment—weight
loss and/or malnutrition often stem from issues that are easily
addressed.
“When they live alone, they often eat alone; and they may eat less.
Or they don’t want to cook for one and will skip meals or eat fewer
balanced meals,” says Marcie Rittenhouse, RDN, CSG, a consultant
dietitian at central Pennsylvania-based LIFE/PACE program. “Some don’t
have family checking in on them regularly, so no one notices at first
when their eating habits change or they start to lose weight.” Even
those elders who live with family can be at risk.
“We have some older people who live with an adult child or other
family member who also eats poorly,” she says. In these cases, an
occupational therapist or social worker can make home visits and
identify issues, such as Mrs. Smith doesn’t know how to use her
microwave, or Mr. Jones needs a way to get to the grocery store.
Sometimes, the solution is as simple as helping to schedule rides to the
store with a neighbor or arranging for the person to participate in a
Meals-on-Wheels program or eat lunch at a local senior center.
Encouraging Elders to Eat
For residents of an assisted living community, they may just need
some encouragement and incentive to go to the dining hall for meals. For
instance, staff can introduce them to other residents who they can eat
and socialize with.
In some instances, a more complex and urgent intervention is
necessary. “Sometimes elders are in dysfunctional family situations that
are affecting their ability to eat well. For instance, they have an
adult child who has an alcohol or drug problem,” says Rittenhouse.
It’s important to realize that people have varying views about and
relationships with food. For instance, Rittenhouse had one patient who
lived with her daughter, who firmly believed that mom should sit at the
table and eat a full hot meal. She was upset because her mother was
resistant. “I had to remind the daughter that her mom is in her 80s and
doesn’t need as many calories or as much food as a younger person,”
Rittenhouse says.
She says another family wanted to use food as a reward or incentive
for certain behaviors. “Food should never be used as a punishment or
reward, and we shouldn’t pressure or force people to eat,” Rittenhouse
says. “We should let them eat when they are hungry, and help ensure that
they get food they enjoy.”
Communicating Choices
Sometimes, it may be difficult for families and caregivers not to
impose their own feelings about food onto an elder. For instance,
Rittenhouse worked with one woman who was emaciated but resisted eating
more because she “likes to stay trim.”
If someone is very thin, Dharmarajan says to do a Body Mass Index
(BMI) test and assess them for any problems. “If there are no red flags
such as an excessively lower BMI, physical weakness, falls, depression,
isolation, or lethargy, we shouldn’t push him or her to eat more,” he
says.
Smith adds, “You must determine whether this is just cultural and
‘normal’ thinking or a psychological disorder, such as anorexia
tardive.” He says that a psychiatric exam might be in order.
To help determine if there is a body image issue that may need to
be addressed, ask patients to clip pictures from a magazine of people
they identify as “too thin,” “thin,” and “obese.” This type of exercise
can be very revealing, he says.
Such personal beliefs, as well as cultural issues and preferences regarding food, should be identified on admission.
“My mother is a lacto-ovo vegetarian, and we made sure the nursing
staff at her facility knew this from the start,” Dharmarajan says. “I
told them that she particularly loves yogurt, which she ate all her
life. But I also told them that she can have anything she wants to eat,
although she has diabetes.” At her stage of advanced dementia, her
quality of life was more important, and avoidance of restrictive diets
was at the top.
Facility staff should meet with families within a few days of
admission to have a care planning conversation that includes a
discussion of food and dietary preferences, including a review of
medications, Dharmarajan says. He also recommends a nutritional
evaluation of the patient on admission to determine if they are
malnourished or at risk for malnutrition. He also recommends a
nutritional evaluation of patients on admission to determine their
nutritional status.
Patients often come from the hospital deconditioned and
malnourished, particularly after a long illness, he says. “We need to
assess them early and determine what needs to be done to help them
recover their strength, regain lost weight, and be as nutritionally
sound as possible given their condition,” he says.
Dietary Restrictions: Less Is More
Clinicians do not generally recommend restricted diets for older
nursing facility residents, particularly those with a life expectancy of
five years or less. “Generally, we allow these patients to eat what
they want,” says Brubaker.
There have been many studies about the value of certain kinds of
diet for cardiovascular and brain health as people age. However, Smith
says, “Nutritional research related to diet and outcomes is fraught with
difficulty, and the methodology for many population-based nutritional
studies is flawed.” Nonetheless, he notes that the Mediterranean diet
has been shown to have some value.
“Here in Texas, the Paleo diet is catching on. The philosophy is to
emulate the diet of our cave-dwelling forefathers with a focus on meat
and vegetables and a de-emphasis on simple carbohydrates and sugars,” he
says.
While a healthy diet for all is ideal, maintaining weight and
strength is a key goal for the elderly, and this often requires
flexibility. “In the not-too-distant past, we were recommending
therapeutic diets for the elderly; then expert opinion determined that
these diets don’t really benefit this patient population because of
their shorter life expectancy,” Smith says. However, he stresses that
restrictive diets are appropriate for younger nursing facility patients.

“While we can’t make them eat healthy, of course, we should always
educate younger patients about why they should or shouldn’t eat
different foods,” Smith says, admitting that this can be challenging
when patients have limited mental capacity or an inability or
unwillingness to hear and retain information.
Dharmarajan stresses the importance of discussing liberalized diets
with family members up front. “If a man had been a diabetic for years
and was on a strict diet, you don’t want his family to see a cookie on
his tray and get upset. You want to help them understand why you are
liberalizing their father’s diet,” he says.
Brubaker agrees that these family discussions are essential. “Some
families are very committed to things such as tight diabetic management.
However, when we talk to them about the benefits of a liberalized diet,
most will understand,” he says.
Are Supplements Super?
“I would rather patients eat food than spend their money on things
like vitamin waters, energy drinks, and vitamin or herbal supplements,”
says Rittenhouse. Another problem with these is that they can be costly.
“We had a woman who was buying $2 bottles of mineral water that she
couldn’t afford, and whatever benefit she might be getting from it
wasn’t worth the cost. We have to consider what is affordable, as well
as what will produce the best outcomes.”
Appetite stimulant medications might seem like a quick fix, but
Smith cautions against them. None is approved by the Food and Drug
Administration for use by the elderly, he says. At the same time, most
appetite stimulants are expensive and have more risks than benefits for
this patient population. It is better to evaluate patients and find the
root cause of weight loss, he says.
Skilled nursing facility patients generally have a need for or can
benefit from nutritional supplementation, such as vitamin D, Smith says.
However, he says, “These patients don’t need more pills, and nurses
don’t need more med passes to make.” One solution might be food
additives, Smith suggests.
“Fortify the ‘real food’ so that it better meets the resident’s
needs. This could be done across the board so all residents get the
benefit. Of course, additives can be individualized to resident needs
when giving something to everyone isn’t appropriate or necessary,” he
says.
How Surveyors See Weight Loss
The prevalence of weight loss is a quality indicator for skilled
nursing centers, and regulations state that facilities must ensure that
residents maintain acceptable parameters of nutritional status, such as
body weight and
protein levels, unless a resident’s clinical condition
demonstrates that it isn’t possible. According to the Investigative
Protocol for Unintended Weight Loss in nursing centers, a more than 5
percent unplanned drop in weight after a month, greater than 7.5 percent
after three months, and 10 percent after six months are considered
“significant” losses.
To help ensure that surveyors understand the reason for unplanned
weight loss, it is important to document regular weights, interventions
taken, and discussions with the patient and/or family members regarding
nutrition and weight.
It is important to document efforts to balance patient choice with
sound clinical care. This isn’t always easy, Smith admits. “I have
encountered surveyors who say that a resident has the right to eat
whatever he or she wants, even if the person’s legal guardian and I both
agree that the resident shouldn’t be able to spend money on candy and
sodas. We have to protect the resident’s rights. But it’s also our
responsibility to take charge of decision-making areas where they lack
capacity.”
“Staff often worry that weight loss will result in survey
citations,” Dharmarajan says. “But surveyors just want to be sure that
patients aren’t losing weight because they aren’t getting enough to eat
or the food is of poor quality.”
It is key to document how weight loss is assessed and addressed;
what care goals related to weight loss are established; and the progress
made on the approach, including conversations about the issue with the
patient and/or family members, he says. This documentation will show
surveyors that staff have identified the problem, are managing it
appropriately, and are respecting the patient’s wishes and
autonomy.
The Trouble with Tube Feeding
Dysphagia,
especially as a patient nears the end of life, often leads to
conversations about tube feeding. “Family members sometimes believe that
a PEG [Percutaneous Endoscopic Gastrostomy] tube will help their loved
one and make him or her feel better,” Dharmarajan says. However, “The
reverse is true. This intervention doesn’t increase life expectancy or
improve quality of life.”
Nonetheless,
family members or decision makers often are influenced by factors such
as misperceptions about feeding and hunger, an inadequate understanding
of the natural course and progression of dementia, lack of understanding
about evidence regarding the risks and benefits of tube feeling, and
cultural or religious beliefs. This is where a good practitioner-family
relationship is so important, he says.
“No tube is placed without informed, educated consent, and this
requires a serious conversation with the patient and/or his family or
decision maker,” Dharmarajan says. The decision about a PEG needs to be
based on understanding and weighing the risks and benefits, not on
presumptions. Undue expectations should not be offered.
In instances where the patient lacks decision-making capacity, has
no living will, advance directive, or designated decision maker,
“Clinicians must assume that a patient wants nutrition therapy until
proven otherwise or until evidence is found to the contrary,”
Dharmarajan says. However, there is much controversy surrounding the
ethics of placing PEGs in patients for whom there is reduced or limited
clinical benefit. This intervention is associated with complications
that may be related to the tube itself, aspiration pneumonia, and
pressure ulcers.
In advanced dementia, PEGs are typically placed to prevent
aspiration and pressure ulcers, improve function, and prolong life
expectancy. However, the risks in reality outweigh the benefits,
Dharmarajan says. For instance, patients can’t move with the tube
inserted, so they become bedbound and susceptible to pressure ulcers,
deconditioning, muscle weakness, and other issues. Also, he notes,
“Converting from hand feeding to a PEG deprives the patient of touch,
taste, nurturing, and social interaction.”
In fact, family members or caregivers often are the ones who gain a
real benefit from a PEG. “The family’s or caregiver’s quality of life
usually improves, as their frustrations may be tempered and they
believe—falsely—that they are preventing their loved one from suffering
due to hunger or thirst, he says.
An honest, open conversation with the family can help clear up
misconceptions. However, this isn’t always the case. “Sometimes, a
family member is insistent, even after being presented with all of the
information and facts,” Brubaker says. “Often this is because they are
dealing with their own feelings about death and dying.”
When this happens, he says, it may be helpful to refocus the
discussion on what their loved one would want. “We need to be aware of
this and try to determine why someone insists on a PEG, even when the
risks outweigh the benefits.”
Sometimes Weight Loss Is Welcome
Obesity is epidemic in the United States, and it is problematic in
nursing centers as well. “We are seeing more obese patients, and they
often have related problems such as diabetes, heart disease, stroke, and
vascular problems,” says Brubaker.
“We can’t expect people to change lifelong habits late in life, but
we can try to reduce caloric intake and have discussions about diet and
nutrition.”
“You won’t perform miracles with obese patients, but we can always
attempt to help them lose some weight and be healthier,” says
Dharmarajan. “This includes trying to get them to be more active, if
possible.” He says it is important to be positive and encouraging and
not make patients feel bad. “Set realistic targets for weight loss, and
always praise the patients for positive behavior.” Help them understand
how weight loss is related to quality of life.
Particularly for younger patients, bariatric surgery might be an
option, Dharmarajan says, but the first approach is always to address
lifestyle: diet and physical activity. Always individualize, taking into
context the individual’s overall illness and life expectancy.
Don’t Wait on Weight
Having the ability to monitor weight and quickly address weight
loss is essential to keep patients as happy and functional as possible
and, importantly, to keep them out of the hospital. “In the hospital,
deconditioning happens remarkably quickly, and many patients come to us
with malnutrition,” says Smith.
Being proactive and staying on top of weights is essential. At the
same time, facilities can be creative about ways to encourage resident
nutrition and healthy weights. For instance, Kings Harbor in New York,
which caters to Indian seniors, has chefs and dietary teams who make
authentic Indian meals. The Lott Residence, also in New York, has its
dining hall on a top floor so that residents can enjoy a breathtaking
view of the city while they eat.
Other facilities have private dining areas where residents can cook
and eat with family members, and many communities offer special meals
and celebrations featuring ethnic and regional foods popular among their
residents.
“Put yourself in your patients’ shoes,” Dharmarajan says. “If you
serve foods I don’t like, I’m not going to eat them. Food is one of
life’s great pleasures, and we need to enable our residents to preserve
this joy for as long as possible.”
Joanne Kaldy is a freelance writer and communications consultant based in Harrisburg, Pa.